How Schizophrenia Symptoms Appear Differently in Teens vs. Adults
Table of Contents
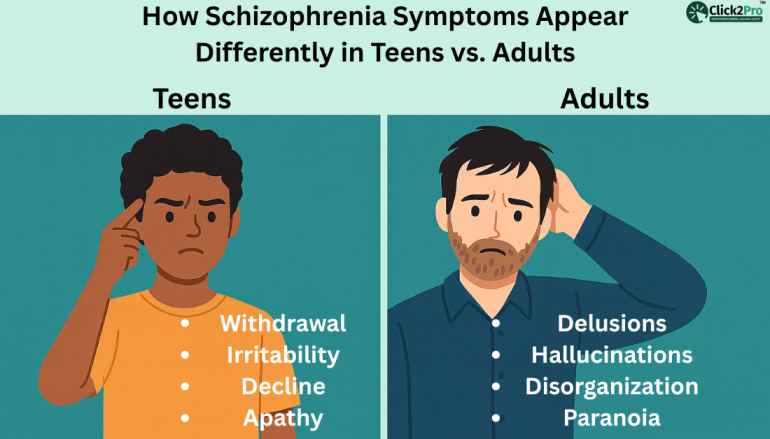
- Why Teen vs. Adult Symptoms Look Different
- Early Schizophrenia Symptoms in Teenagers
- Schizophrenia Symptoms in Adults
- Direct Comparison: Teens vs. Adults
- Global Statistics for Schizophrenia (U.S., India, UK, Australia, Canada, UAE)
- Causes & Risk Factors
- Diagnosis Challenges: Teens vs. Adults
- Treatment Approaches for Teens vs. Adults
- Real-World Stories
- When to Seek Help
- Cultural Influences & Family Dynamics
- Future Trends in Schizophrenia Understanding
- FAQs
- About the Author
Why Teen vs. Adult Symptoms Look Different
Schizophrenia does not appear the same at every age. The brain changes rapidly during the teen years, which is why symptoms often look scattered, confusing, and even invisible at first. Adults, on the other hand, show clearer symptom patterns because their emotional and cognitive systems are more developed. This difference is one of the biggest reasons families from the U.S., India, the UK, Australia, Canada, and the UAE often miss early signs in teenagers until the condition feels overwhelming.
Snippet-Ready Insight:
Schizophrenia symptoms look different in teens because their brain is still developing, emotions shift quickly, and normal adolescent behavior can hide early warning signs.
During adolescence, the prefrontal cortex is still under construction. This area manages judgment, planning, emotional control, and social decision-making. When schizophrenia begins at this stage, its subtle early symptoms blend into common teenage behavior. A teen who becomes withdrawn may appear to be “just moody.” A student who suddenly loses interest in school might seem bored. Parents think the changes are normal, and teens rarely talk about unusual experiences because they don’t yet understand them.
Cultural expectations also shape how symptoms are recognized. In the U.S. and Australia, teens are encouraged to talk about mental health, yet long wait times and limited access in rural states cause delays. In India, silence around mental illness still pushes many families to hide early symptoms until they become disruptive. In the UK, early intervention teams exist, but many teens avoid seeking help, fearing judgment from classmates. These cultural layers matter because schizophrenia relies on early identification for better outcomes.
Adults show clearer red flags because they have a stable baseline. Their work, responsibilities, and daily routines make sudden changes easier to notice. When an adult begins hearing voices or believes someone is watching them, family members tend to identify the shift more quickly. Adults also describe their inner experiences with greater clarity. Teenagers often can’t do this yet. They may not know how to explain frightening thoughts or strange sensations.
The brain’s maturity is not the only factor. Hormonal changes, sleep disruptions, academic pressure, and social conflicts during teenage years add noise to the picture. Because of this, teen symptoms are often misdiagnosed as depression, ADHD, bipolar disorder, or simple rebellion. Adults are more likely to be diagnosed accurately on the first evaluation.
These differences matter for global mental health understanding. Families in the UAE and Canada report that adult symptoms look more structured-consistent delusions, organized hallucinations, and noticeable withdrawal from social roles. Teen symptoms, in contrast, appear chaotic and unpredictable. This contrast is the reason mental-health professionals across countries approach teen assessments differently from adult assessments.
Early Schizophrenia Symptoms in Teenagers
Teen schizophrenia symptoms are often quiet at first. They rarely start with the dramatic hallucinations people imagine. Instead, they slip into a teen’s life slowly, affecting their mood, focus, energy, and social behavior. Many families say things “felt off” months or even years before a diagnosis, but nothing seemed serious enough to act on. That delay is common in the U.S., Canada, and Australia, where school pressure and teenage stress mask early signs. In India and the UAE, cultural hesitation adds another layer that delays help even further.
Snippet-Ready Insight:
Early schizophrenia symptoms in teenagers often appear as subtle behavior changes-withdrawal, unusual fears, academic decline, sleep shifts, or unexplained irritability-far before hallucinations or delusions begin.
One of the earliest signs in teens is a decline in functioning. A teen who once enjoyed sports or art may suddenly lose interest. Grades start to drop, friendships fade, and the teen may spend long hours alone. Instead of seeking company, they feel safest tucked away in their room. When asked, they might say they’re “tired” or “not in the mood.” Parents interpret it as stress or puberty. However, early schizophrenia often shows itself through this slow retreat from life.
Another early symptom is changes in thinking. Teens may struggle to follow conversations or lose track of what they’re saying. Their thoughts feel tangled. They pause often or switch topics abruptly. Many describe it as “my brain feels foggy.” This cognitive disruption is a key early sign, yet it is commonly mistaken for distraction or lack of motivation.
Emotional changes also appear early. Teens may show flat or unpredictable emotions. A teen who once laughed easily may seem emotionally distant. Another might react with sudden bursts of anger or anxiety without clear reasons. In multicultural societies like the U.S., UK, and UAE, families sometimes confuse these shifts with teenage mood swings. But in early schizophrenia, these changes persist for weeks or months.
Sensory sensitivities provide another clue. Some teens become unusually sensitive to noise, bright lights, or crowded spaces. A busy classroom or shopping mall overwhelms them. This sensitivity often appears before clear psychotic symptoms.
Behavioral oddities can also emerge. Teens might develop unusual habits, speak in a strange tone, become paranoid about friends, or show fear of being watched. Instead of hallucinations, early paranoia looks like mistrust and social withdrawal. This can be misunderstood as anxiety or the impact of bullying.
Sleep changes are another quiet sign. Teens with developing schizophrenia may stay up all night, sleep excessively, or reverse their sleep schedule. Lack of sleep worsens their thinking and emotions, making symptoms harder to untangle.
Family reports from India, the UK, and Australia often include something else: a noticeable decline in self-care. Teens may forget to shower, wear the same clothes for days, or appear disheveled. They might say they “don’t feel like it,” but deeper disruptions in motivation and focus are usually happening beneath the surface.
Professional experience also shows that teens rarely admit when something feels wrong. They fear being judged. They think others will call them crazy or dramatic. Some don’t understand that their inner experiences are unusual. Because of this, early symptoms stay hidden until they become severe enough to disrupt daily functioning.
Snippet-Ready Insight:
Teens with early schizophrenia often appear overwhelmed, withdrawn, forgetful, or unusually anxious long before delusions or hallucinations are noticeable.
These early signs are not a diagnosis. They are signals that something more complex may be happening beneath typical teenage behavior. Understanding them early brings families one step closer to support, clarity, and better long-term outcomes.
Schizophrenia Symptoms in Adults
When schizophrenia appears in adults, the symptoms look clearer and more structured than they do in teenagers. Adults usually have a stable routine, a defined personality, and predictable patterns in work or relationships. Because of this, sudden changes stand out more sharply. Families often tell me they noticed a shift “almost overnight,” even though the condition develops slowly beneath the surface. The visible difference happens because adults have already crossed key stages of brain development, identity formation, and emotional maturity.
Snippet-Ready Insight:
Adults with schizophrenia show more organized symptoms-clear delusions, persistent hallucinations, and noticeable thinking problems-because their brains and behaviors are more stable and easier to compare to their usual selves.
The most recognized adult symptom is the development of well-formed delusions. A person may believe someone is watching them, plotting against them, or sending hidden messages. These beliefs feel real to them. Adults can explain these thoughts in detail, which helps clinicians identify the problem sooner. Teens often cannot explain their thoughts this clearly.
Hallucinations are also more defined in adults. Many adults describe hearing voices that comment on their actions, argue with each other, or speak directly to them. Adults find this distressing and try to hide it at first. When it becomes harder to manage, families notice changes such as talking to themselves, reacting to unheard voices, or appearing lost in thought during conversations.
Another early adult symptom is cognitive disruption. Adults may forget simple tasks, lose track of time, or struggle with decisions they once made easily. A manager who handled projects well may suddenly fall behind. A parent who used to run the household might become confused by basic tasks. These declines are easier to observe because adults typically have established responsibilities.
Emotional changes appear too. Adults may show little expression, even during important moments. Some stop reacting to good news or sad events. Others become anxious, irritable, or suspicious without obvious reasons. Families from countries like India and the UAE often interpret these shifts as stress or life pressure, especially if the person works long hours. In the U.S., Canada, and Australia, these signs may be mistaken for burnout or depression.
Social withdrawal is another red flag. Adults may stop spending time with family, avoid friends, or lose interest in activities they once enjoyed. A lively person becomes quiet. A social adult avoids gatherings. They might feel safer alone because their inner world becomes louder than the outside one. This withdrawal is often misread as introversion or exhaustion, which delays support.
Behavioral changes also develop. Adults may speak in fragmented sentences, have difficulty organizing thoughts, or jump rapidly between topics. Some begin collecting unnecessary items or repeating certain actions. These behaviors appear odd but not always alarming at first.
Daily functioning is affected too. Adults may stop maintaining personal hygiene or neglect their home. Dishes pile up. Bills go unpaid. The person may appear overwhelmed by simple tasks. In multicultural settings like the UK and Australia, families might assume it stems from depression until more severe symptoms appear.
Adults usually have more insight compared to teens. They sense something is wrong, even if they cannot describe it clearly. Some reach out for help, saying they feel “disconnected” or “not themselves.” Others hide their symptoms out of fear or shame. The stigma remains strong in many parts of the world, especially in South Asian communities where mental illness is often misunderstood.
These adult symptoms, while distressing, provide clearer clues for early recognition. The structure of adult life makes shifts easier to identify, which can lead to faster assessments. Unlike teens, adults rarely blend schizophrenia symptoms with normal life transitions, making it easier for professionals to understand the pattern.
Direct Comparison: Teens vs. Adults
The clearest way to understand schizophrenia is to compare how it appears at different ages. The contrast between teen and adult symptoms is not just a difference in intensity. It reflects brain development, life experience, responsibilities, and the environments people live in. When families understand this difference, they can spot concerns earlier and seek guidance without assuming the behavior is “just growing up” or “just stress.”
Snippet-Ready Insight:
Teen schizophrenia symptoms are subtle, scattered, and often mistaken for normal behavior, while adult symptoms are organized, intense, and easier for others to recognize.
Teens experience symptoms that blend into everyday adolescent struggles. Their behavior is already shifting due to hormones, school pressure, identity changes, friendships, and uncertainty about the future. Because of this, early schizophrenia can look like typical teenage behavior. A student’s sudden drop in grades may be dismissed as laziness. A teen’s desire to stay alone may be seen as a phase. When symptoms hide behind normal behavior, recognition becomes difficult.
Adults show more consistent patterns. A professional who has always been punctual suddenly missing deadlines sends a noticeable signal. A parent who used to handle responsibilities smoothly becomes confused by daily tasks. These changes are easier to measure because adults usually live predictable lives. When that rhythm breaks, people notice the difference.
Emotionally, teens often appear overwhelmed or unpredictable. They may react strongly one day and appear flat the next. Adults show a more stable pattern of emotional flattening. They become quieter, more withdrawn, or suspicious with less fluctuation. This creates a clearer clinical picture.
Delusions and hallucinations differ too. Teens have trouble describing what they experience. They may say, “I feel weird,” “Someone doesn’t like me,” or “People are confusing me.” Adults express clearer beliefs. They might describe hearing voices or sensing danger that others don’t see. Because adults can explain their inner experiences, clinicians can identify symptoms with more accuracy.
Cognitive symptoms also diverge. Teens may appear forgetful, distracted, or confused, which is easy to blame on school pressure or lack of focus. Adults show sharper cognitive decline. They might struggle to organize their tasks, balance simple decisions, or manage their day. In countries like the U.S. and Canada, this often affects workplace performance, which becomes difficult to hide.
Cultural context adds more contrast. In India and the UAE, teenage behavior is sometimes controlled closely by family members. Because of this, symptoms may appear as disobedience rather than early psychosis. Adults, however, face expectations at work and home. When those expectations are not met, the family starts to notice something deeper happening. In the UK and Australia, where mental-health awareness is more accessible, the differences between teen and adult symptoms are recognized faster, although stigma still delays conversations.
Insight is another distinction. Teens often cannot understand or articulate what is happening. Their brain is still learning to interpret emotions and thoughts. Adults usually sense that something is wrong. They may feel frightened, disconnected, or confused by their own thoughts. This awareness helps professionals reach a diagnosis earlier.
Functioning patterns also reveal important differences. Teens rely on parents, teachers, and school routines. When their functioning changes, adults may assume they need discipline or motivation. Adults rely on themselves. When functioning drops, the impact is immediate: job instability, relationship strain, financial problems, or social withdrawal. Because these consequences are visible, adult symptoms are harder to ignore.
Overall, schizophrenia unfolds differently because teens and adults occupy different stages of life. Teens are building their identities, and symptoms blend into that process. Adults have established identities, and symptoms disrupt what is already built. Understanding this comparison strengthens early recognition and reduces the emotional burden on families.
Global Statistics for Schizophrenia (U.S., India, UK, Australia, Canada, UAE)
Schizophrenia affects people across the world, but the way it shows up, gets recognized, and gets talked about varies by culture, access to care, and awareness. The global prevalence sits close to one percent, yet the burden feels much heavier in countries where mental-health care is limited or stigma silences early symptoms. Understanding these numbers helps families realize that schizophrenia is not rare, not a sign of weakness, and not a moral failure. It is a condition that appears in every country, culture, and lifestyle.
Snippet-Ready Insight:
Schizophrenia affects roughly one percent of the global population, with millions of people living with it across the U.S., India, Canada, the UK, Australia, and the UAE.
In the United States, millions of people live with schizophrenia, making it one of the leading chronic mental-health conditions. Large states with dense populations, such as California, Texas, and New York, report higher numbers of diagnosed individuals. This is partly due to larger mental-health networks that identify cases earlier. Rural areas, however, face long delays in diagnosis and limited treatment access.
India shows a significant number of cases as well. With its massive and diverse population, estimates fall in the several-million range. Urban cities like Delhi, Mumbai, Bengaluru, and Kolkata record higher detection rates because psychiatric services are more available. Rural states often see late diagnosis because families hide symptoms or lack access to professionals. Stigma plays a strong role. Many families wait until symptoms disrupt schooling or work before seeking help.
The UK reports close to one percent prevalence as well. Cities like London, Manchester, and Birmingham have strong early intervention teams, which increases detection. Yet, even in the UK, delays happen when symptoms blend into stress, grief, or burnout. Awareness is higher than in many countries, but fear of judgment still causes hesitation.
Australia also reports a similar range, and its youth-focused mental-health services have helped detect schizophrenia earlier in young adults. Cities like Sydney, Melbourne, and Brisbane have structured programs, while remote regions face challenges due to distance. Teens and adults in rural areas may miss early assessments because mental-health professionals are limited.
Canada has comparable rates, with provinces like Ontario, British Columbia, and Quebec reporting higher numbers simply due to population size. Early intervention programs are more visible in urban areas, yet families in smaller towns often struggle to find consistent support.
In the UAE, the number of identified cases has grown as awareness rises. Mental-health stigma still influences how quickly families seek help, especially when symptoms appear in teenagers. However, major cities like Dubai and Abu Dhabi have improved services, allowing earlier assessments and reduced delays.
These global statistics show a consistent truth. Schizophrenia is not country-specific. It does not belong to one culture or one demographic group. It crosses borders, languages, and lifestyles. What changes is how quickly people talk about it, how easy it is to get support, and how families understand early signs. This global lens helps normalize the condition and encourages families to trust their observations rather than wait for symptoms to escalate.
Causes & Risk Factors
The causes of schizophrenia are complex, and no single factor explains why it appears earlier in some people and later in others. What we do know is that genetics, brain development, environment, and life stress interact in different ways depending on age. This interaction shapes how schizophrenia begins in teens and adults, and it influences how symptoms unfold over time. Understanding these risk factors helps families recognize that schizophrenia is not a choice, not a failure, and not caused by personal weakness.
Snippet-Ready Insight:
Teen schizophrenia is more influenced by brain development, genetics, and early life factors, while adult-onset cases are more connected to long-term stress, social isolation, and accumulated risks.
Teenage schizophrenia is strongly tied to neurodevelopment. The brain goes through rapid growth during adolescence, especially in areas responsible for thinking, planning, and emotional regulation. When changes disrupt this process, symptoms may appear earlier. Teens who have a family history of mental-health conditions are more vulnerable because inherited traits play a role. Early life complications, such as stress during childhood, trauma, or medical complications during birth, can also increase risk. These factors do not guarantee schizophrenia. They simply create a more sensitive environment within the developing brain.
Substance use is another age-specific factor. Teen brains react more strongly to substances like cannabis or stimulants. Some teens use them to cope with school pressure, friendships, or emotional discomfort. When vulnerability already exists, these substances can accelerate the onset of symptoms. This pattern is seen in many countries, including the U.S., Canada, the UK, and Australia, where substance access is relatively common. Families often report that symptoms became noticeable after changes in social circles or experimentation with substances.
Stress plays a large role in teen schizophrenia as well. Academic pressure, shifting friendships, bullying, identity struggles, and social media influence can increase emotional strain. Teens do not always express stress clearly. They often hide it or minimize it. This silence makes early symptoms harder to track.
Adult-onset schizophrenia has its own set of risk factors. Long-term stress builds slowly. Years of emotional strain, social isolation, financial pressure, or personal loss can contribute to the development of symptoms. Adults who carry genetic vulnerability may not show signs until life stressors push the system into overload. Many adults describe a slow unraveling of their ability to cope before symptoms become visible.
Chronic substance use can also contribute to adult-onset cases. While teens may experience rapid changes, adults often face a longer buildup. Continued use of alcohol or drugs can amplify existing vulnerabilities. This pattern is seen across the U.S., India, and Australia, where adults may use substances to manage work stress or emotional pressure.
Brain aging plays another role. Even though schizophrenia is not caused by aging, certain changes in cognitive control and emotional resilience can influence how symptoms begin. Adults may feel their thinking becoming foggy or disorganized long before clear symptoms appear.
Cultural and environmental factors also shape risk. In India and the UAE, social expectations and stigma may force adults to suppress their emotional struggles. In the U.S. and UK, isolation and long work hours can increase vulnerability. In Australia and Canada, geographic distance and limited services in remote areas create delayed recognition.
The interaction between these factors is what matters. No single cause explains schizophrenia. It emerges from a combination of genetic sensitivity, emotional history, environmental pressure, and brain development. What differs is the timing. Teens experience symptoms earlier because their brains are still forming. Adults experience symptoms when accumulated stress triggers underlying vulnerabilities.
Diagnosis Challenges: Teens vs. Adults
Diagnosing schizophrenia is difficult at any age, but the challenges multiply when the symptoms appear during adolescence. Teens are already changing rapidly. Their emotions shift, their social circles evolve, and their thinking patterns stretch as they grow. These changes make it hard for families and professionals to separate ordinary behaviors from early warning signs. Adults, however, live more structured lives. Their routines, responsibilities, and personality patterns make sudden shifts easier to notice. This difference creates gaps and delays in diagnosis that vary across countries and cultures.
Snippet-Ready Insight:
Teen schizophrenia is harder to diagnose because symptoms overlap with normal adolescent behavior, while adults show clearer and more distinct changes.
For many teens, the first signs show up as mood swings, irritability, school resistance, or withdrawal. These are also common teenage behaviors. Teachers may think the student is stressed. Parents may assume the teen is avoiding homework or struggling with friendships. Because the symptoms blend into typical development, early schizophrenia can go unnoticed for months or years.
In the U.S. and Canada, teens often hide unusual thoughts out of fear that others will judge them. In India, families may explain symptoms as misbehavior or lack of discipline. The UK and Australia offer structured youth mental-health services, but even there, many teens hesitate to talk openly about internal changes. These cultural responses influence how quickly professionals can evaluate symptoms.
Adults face different challenges. They recognize that something feels wrong, even if they cannot describe it clearly. They may notice their thoughts becoming disorganized, or daily tasks feeling harder than before. Family members spot changes faster because they interrupt work, relationships, and responsibilities. A person who always paid bills on time suddenly forgets. Someone who handled stress well may become overwhelmed by simple tasks.
Despite clearer symptoms, adults still face delays. Many assume their changes are caused by stress, burnout, or relationship issues. In fast-paced environments like New York, London, Dubai, and Mumbai, adults often blame symptoms on pressure rather than something deeper. This delays early assessment.
Teen diagnosis involves more observation. Professionals must speak with parents, teachers, and the teen. They explore behavior at school, home, and with friends. Adults, meanwhile, can explain their inner experiences in more detail, which helps clinicians understand the pattern sooner.
Misdiagnosis is common in both groups but for different reasons. Teens may be labeled with ADHD, depression, or anxiety, because early schizophrenia affects motivation and focus. Adults may be misdiagnosed with bipolar disorder or severe depression. Without a full understanding of the person’s history, the early stage can look like many other conditions.
Another challenge is stigma. Teens fear being “different,” and adults fear losing stability. In India, the UAE, and some South Asian communities, stigma prevents families from speaking openly. This silence blocks early detection. In Western countries, fear of job loss or relationship strain has a similar effect on adults.
Diagnosis becomes easier when families notice patterns instead of isolated moments. Teens who consistently withdraw, lose interest, or show unusual fears deserve attention. Adults who suddenly change their habits or express unusual beliefs deserve the same care. Understanding these differences brings clarity to families across cultures and helps reduce the confusion that often surrounds early symptoms.
Treatment Approaches for Teens vs. Adults
Treatment for schizophrenia varies depending on age, life stage, family involvement, and the environment a person lives in. Teens and adults do not respond to care in the same way because their needs are different. Teens rely heavily on family guidance, school support, and social structure. Adults manage work, relationships, finances, and independent living. These differences shape the way professionals create support plans.
Snippet-Ready Insight:
Teen treatment focuses on family support, school adjustments, and emotional guidance, while adult treatment focuses on independence, stability, and long-term management.
Treatment for teens often begins with building a supportive environment. Families play a central role. Teens need stability and reassurance because their sense of identity is still developing. Therapy focuses on helping them understand their emotions, manage stress, and rebuild academic confidence. School systems become part of the support network. Teachers may adjust workloads or help the teen re-engage with learning. Teens benefit from routines, structure, and clear communication.
Another age-specific focus is social development. Teens are navigating friendships and learning how to communicate. Early schizophrenia affects these areas deeply. Professionals may work with the teen on social skills, self-awareness, and emotional expression. Many teens also need guidance in understanding what is happening to them. They may feel confused, embarrassed, or scared. Gentle education helps reduce fear and encourages open communication.
Adults follow a different path. Their treatment centers on restoring stability and supporting their responsibilities. Some adults need help returning to work or managing daily tasks. Others need guidance in building routines that reduce stress. Therapy often focuses on problem-solving, emotional regulation, and understanding symptoms. Adults benefit from consistent support but also value independence. Treatment helps them maintain that independence while improving coping skills.
Family involvement is still important for adults, but in a different way. Adults may rely on spouses, siblings, or close friends for emotional support. However, they often manage their own decisions, finances, and schedules. Treatment respects their autonomy while offering tools to navigate challenges. In cultures like India, the UAE, and parts of Canada, family involvement remains strong. In Western countries, adults often prefer private, individualized approaches.
Both teens and adults benefit from lifestyle structure. Regular sleep, reduced stress, and stable routines support emotional balance. Teens rely on families and schools to create this structure. Adults build it themselves, sometimes with professional guidance. Because adults face work pressure, financial responsibilities, and relationship commitments, they may require different strategies to manage daily stress.
Access to services also differs across countries. In the U.S., cost and insurance barriers influence treatment choices. In the UK and Australia, public systems provide structured programs. India’s major cities offer expanding mental-health services, while rural areas face shortages. The UAE has invested in modern mental-health facilities, but stigma still affects help-seeking behavior.
The goal for both age groups is not to “cure” symptoms but to strengthen coping skills, improve functioning, and support long-term stability. Teens need reassurance, understanding, and structured guidance. Adults need respect, autonomy, and consistent support. When treatment aligns with age-specific needs, families often see improvements in communication, confidence, and overall quality of life.
Real-World Stories
Real-life experiences often reveal what statistics cannot. They show the confusion, hesitation, and emotional weight families carry when schizophrenia begins. The stories below are composites based on common patterns I’ve seen across different countries. They protect privacy while reflecting the reality many families face. Each story highlights how schizophrenia appears differently in teens and adults, and how life context changes the way symptoms unfold.
Snippet-Ready Insight:
Real stories show that early schizophrenia symptoms often appear subtle, confusing, and easy to overlook in both teenagers and adults.
Case Story 1: A Teen in California Who Slowly “Disappeared” into Isolation
A 15-year-old student from California began to withdraw from her friends one school year. She stopped eating lunch with them and spent most of her time alone in the library. Her parents assumed she was overwhelmed by her classes. Teachers thought she was shy. Over time, she lost interest in the activities she once loved.
Her parents noticed she became sensitive to noise. Crowded rooms made her anxious. She struggled to explain why. When asked, she simply said she felt “off.” Her grades dropped, and she argued more with her siblings. None of the symptoms felt severe enough to signal a major problem. They felt like teenage stress. Months later, she admitted that she sometimes felt watched in school hallways, even when no one was around. Her early symptoms hid behind normal teenage behavior until they became impossible to ignore.
Case Story 2: A Teen Boy from India Misunderstood as “Rebellious”
In a large city in India, a 17-year-old boy started refusing to attend school. His parents thought he was being defiant. They pushed him harder, assuming discipline was the answer. Over time, he became fearful at night, convinced that strangers were talking about him outside. His family misunderstood these fears as excuses.
Cultural stigma played a strong role. His relatives believed he needed motivation, not understanding. Months passed before his parents realized the changes were not intentional. By the time they sought help, his symptoms had grown stronger. His story reflects how cultural expectations can delay recognition in teens.
Case Story 3: A Working Professional in London Who Could No Longer Keep Up
A woman in her early thirties living in London had always managed her work well. One year, she began missing deadlines. She forgot tasks she had done for years. Her coworkers noticed she seemed distracted. She often paused mid-sentence as if she had lost her train of thought.
At home, she withdrew from her friends. She stopped returning calls and felt safer staying alone. Her partner noticed she seemed afraid of shadows or movements she could not explain. Unlike teens, she recognized that something was changing. She described a growing sense of confusion. Because adults have clearer routines, her symptoms stood out early.
Case Story 4: A Young Adult in Australia Who Thought It Was Burnout
A 26-year-old man from Melbourne assumed his symptoms came from work stress. He felt mentally exhausted, avoided social gatherings, and struggled with simple decisions. He told himself it was temporary. Weeks later, he started believing coworkers were whispering about him. He could not explain why but felt certain of it.
His friends thought he needed a break. He believed he just needed rest. Because young adults often blame stress for cognitive changes, his early symptoms blended into everyday life pressure. Only when things escalated did he begin to question what was happening.
Case Story 5: An Adult in the UAE Who Hid His Fears for Years
A man in his mid-thirties from Dubai worked long hours and supported a large family. He started sensing that people were following him. He felt watched in parking lots and elevators. He hid these fears because he did not want his family to worry. In his culture, mental-health discussions were not common. His silence delayed understanding for years.
These stories show how schizophrenia can hide behind ordinary life transitions. They highlight how culture, family expectations, and age influence the way symptoms appear and how quickly they are recognized. They also show how families across the world face similar confusion, regardless of their background.
When to Seek Help
Recognizing the right time to seek help can be difficult. Families often second-guess themselves. Teens and adults often hide their struggles. Friends think it’s stress. Teachers think it’s burnout. Employers think it’s pressure. Because schizophrenia appears gradually, the early signs can feel uncertain. The decision to seek help becomes easier when people understand what consistent, noticeable changes look like.
Snippet-Ready Insight:
Seek help when behavior changes last several weeks, affect daily functioning, or make the person feel disconnected, overwhelmed, or fearful without clear reasons.
For teens, help should be considered when the changes do not fit their usual personality. A quiet teen becoming quieter is normal. A social teen suddenly avoiding everyone for weeks is not. A single bad grade is typical. A steady decline across subjects signals something deeper. Emotional shifts that linger-fear, withdrawal, irritability-are worth discussing with a trusted adult or mental-health professional.
Parents should pay attention when teens describe unusual experiences. Many teens hesitate to share these thoughts. They fear judgment or misunderstanding. When they do speak, even briefly, it is important to listen. Confusion, fear, or difficulty explaining what they feel are strong reasons to explore further guidance.
Adults should consider help when daily functioning changes. A person who handled responsibilities confidently but now feels overwhelmed by simple tasks may need support. Memory problems, unusual fears, withdrawal, or difficulty concentrating are not signs of failure. They are signals that the person is facing internal challenges. Adults often try to push through these changes, but early attention reduces the emotional burden.
Emotion plays a key role in both age groups. Persistent sadness, fear without cause, sudden irritability, or emotional numbness deserve attention. When emotions shift dramatically and stay that way, it means something is happening beneath the surface.
Behavioral changes also matter. Teens or adults who begin isolating themselves, staying in their rooms for long hours, or avoiding eye contact may be struggling internally. A person who becomes sensitive to noise, light, or crowds may be overwhelmed by sensory changes. A pattern matters more than isolated moments.
Families across the U.S., India, the UK, Australia, Canada, and the UAE often wait too long because they fear overreacting. They think things will improve on their own. Sometimes they do, but sometimes they do not. It is safer and kinder to explore concerns early rather than wait for symptoms to escalate.
Seeking help does not mean diagnosing or labeling. It means understanding, listening, and giving the person space to express their experiences. It creates a safe environment where concerns are taken seriously and addressed with compassion. The earlier families pay attention to consistent changes, the easier it becomes to provide meaningful support.Many families today are turning to online counselling in India to understand early emotional changes in teens and adults, especially when subtle symptoms raise questions or create confusion.
Cultural Influences & Family Dynamics
Schizophrenia does not exist in a vacuum. It lives inside families, cultures, and belief systems. The way people understand symptoms in the U.S. is not the same as in India or the UAE. The support systems in Canada feel different from those in the UK or Australia. Culture shapes reactions, interpretations, and the speed at which families seek help. In many cases, cultural responses influence the course of the condition as much as the symptoms themselves.
Snippet-Ready Insight:
Culture shapes how families interpret early schizophrenia symptoms, how quickly they seek help, and how supported the person feels during the process.
In the United States, awareness is higher, but access barriers still exist. Many families recognize behavioral changes early, yet long wait times, high costs, and limited insurance coverage delay assessments. American teens often hide symptoms because they fear being judged at school. Adults fear losing employment or independence. These concerns influence the language families use when discussing changes.
In India, the picture is more complex. Many families view emotional changes through social or spiritual lenses. A teen who becomes withdrawn may be seen as stubborn rather than struggling. Adults may be told to “be strong” rather than explore what they feel. Stigma remains one of the biggest barriers. The desire to protect family reputation sometimes delays help. At the same time, strong family bonds mean many people receive ongoing support once the situation is understood.
The UK offers structured services, and mental-health awareness is widely promoted. Even so, many families hesitate. British teens may worry about being labeled or misunderstood by peers. Adults often hide symptoms out of fear that colleagues may think they are unreliable. Although services exist, early conversations still depend heavily on family understanding.
Australia and Canada share a similar environment. Awareness is growing, and youth programs offer early guidance. Rural areas, however, face significant shortages. Families often try to handle symptoms alone because services are far away. Teens in remote regions may not speak openly about their fears because they worry about social judgment. Adults may avoid discussing symptoms to prevent workplace complications.
In the UAE, cultural expectations and privacy concerns influence how families talk about mental health. Many prefer to keep emotional struggles within the household. Teens fear disappointing their families. Adults fear long-term stigma. However, the country has invested heavily in mental-health resources, and awareness is improving.
Family dynamics deepen these cultural layers. Families that communicate openly tend to recognize early symptoms faster. Families that avoid emotional conversations may miss subtle signs. A teen who feels safe sharing unusual thoughts will be understood sooner. An adult who feels supported will speak earlier about changes they notice.
Culture also affects expectations. In India, teens often face pressure to perform academically. In the U.S., they face pressure to fit in socially. In the UK, mental health is discussed openly, but many still fear judgment. In the UAE, family honor plays a strong role. Each of these pressures shapes how symptoms appear and how individuals respond to them.
Understanding cultural influences does not mean blaming the family or community. It means recognizing the context in which symptoms unfold. When families understand how culture shapes their reactions, they approach symptoms with more compassion and clarity. This awareness becomes a powerful tool in navigating schizophrenia at any age.
Future Trends in Schizophrenia Understanding
The future of schizophrenia research and understanding is shifting rapidly. Scientists, psychologists, and clinicians are uncovering new insights that help explain why the condition appears differently across ages and cultures. These trends offer hope, clarity, and new directions for families who want to understand the condition better. While the exact causes remain complex, the research points toward patterns that make early recognition easier and support more personalized care.
Snippet-Ready Insight:
Future research is moving toward early detection, personalized care, and a deeper understanding of how brain development affects schizophrenia at different ages.
One major trend is the focus on early detection. Researchers are studying how brain development interacts with life experiences in teens. Understanding these changes helps predict when symptoms may appear. Behavioral shifts, cognitive patterns, and emotional markers are being studied in younger groups to identify early risk signals. This research gives hope for earlier support long before symptoms become disruptive.
Another trend is the integration of lifestyle and emotional factors into symptom interpretation. Instead of relying only on structured interviews, professionals are exploring how sleep patterns, life stress, academic pressure, and social connections influence early symptoms. This holistic approach reflects the real-world experiences of teens and adults from different cultures.
The role of stress is also gaining attention. Chronic pressure in adults is being studied as a trigger for symptoms in individuals who already carry vulnerability. This trend helps explain why some adults develop symptoms after long periods of emotional strain. It also highlights the need for supportive environments, balanced routines, and open communication.
Cultural understanding is becoming central to future research as well. Experts now acknowledge that schizophrenia looks different depending on the beliefs, expectations, and resources available in each country. Teens in India may show different coping patterns than teens in the U.S. Adults in the UAE may describe their symptoms differently than adults in Canada. Because of this, more global research models are emerging. These models study symptoms within cultural contexts, not outside them.
There is also growing interest in understanding life transitions. Adolescence and early adulthood are now recognized as sensitive stages where the brain is both vulnerable and adaptable. Research is exploring how identity, emotional maturity, and social stress shape symptoms. This helps explain why teen symptoms look scattered and adult symptoms look more structured.
Future studies are also moving toward personalized care. Instead of using one approach for everyone, professionals analyze each person’s history, lifestyle, emotional needs, and cultural background. Personalized approaches can make support systems more effective and less intimidating.
Technology is another growing trend. Digital tools are being developed to help families track changes in behavior, sleep, and mood. These tools do not diagnose but help families understand patterns. They create a timeline that makes conversations easier and more accurate.
The future of schizophrenia understanding is not only about science. It is about empathy. It is about giving teens and adults the language to describe their experiences. It is about equipping families with knowledge so they feel less afraid. And it is about shaping societies where emotional struggles are viewed with compassion rather than judgment.
FAQs
1. What are the earliest signs of schizophrenia in teens?
Early signs often appear as small, quiet changes. Teens may withdraw from friends, lose interest in hobbies, or fall behind in school. Some become sensitive to noise or light. Many feel overwhelmed but cannot explain why. These early changes last for weeks or months, not just a few days.
Snippet-Ready:
The earliest signs in teens look like isolation, fear, academic decline, and emotional shifts that do not fit their usual personality.
2. How do schizophrenia symptoms differ between teens and adults?
Teen symptoms blend into normal growing-up changes. They show confusion, irritability, and withdrawal before clear hallucinations appear. Adults show more structured symptoms, such as organized delusions, persistent hallucinations, and noticeable changes in thinking.
Snippet-Ready:
Teens show subtle, scattered symptoms; adults show clearer, well-defined symptoms.
3. Can schizophrenia start at age 14 or younger?
Yes. Early-onset schizophrenia can appear between 13 and 18. Symptoms tend to be milder at first and harder to recognize because teen behavior varies so much.
4. Are hallucinations common in teenagers with schizophrenia?
They can happen, but teens rarely describe them clearly. Instead of saying they hear voices, they may look distracted, anxious, or confused. Parents often notice behavior changes long before hallucinations are mentioned.
5. How can parents tell the difference between teenage moodiness and early schizophrenia?
Look for patterns, not moments. Moodiness comes and goes. Early schizophrenia creates consistent changes that last, such as withdrawal, fear, poor focus, or unusual behavior. When these changes persist for weeks, it’s worth discussing with a professional.
6. Why are teenagers often misdiagnosed?
Teen symptoms overlap with depression, anxiety, ADHD, and trauma. Because teens have limited emotional language, they struggle to explain what they feel. This leads to confusion during early evaluations.
7. Does schizophrenia progress faster in teens?
Teens may show faster changes during stressful periods, but it does not mean the condition always progresses quicker. The symptoms appear earlier because the brain is still developing.
8. Can adults suddenly develop schizophrenia?
Yes. Many adults first experience symptoms in their late 20s or early 30s. Stress, emotional strain, and genetic vulnerability can influence the timing, but the shift can feel sudden to the person and their family.
9. How long does early psychosis usually last?
The early phase can last months or even years. Teens often experience a longer early phase because their symptoms blend into typical behavior. Adults may notice their early phase more quickly because responsibilities make changes easier to spot.
10. Can stress alone cause schizophrenia?
Stress does not create schizophrenia by itself. It can trigger symptoms in someone already vulnerable. Teens and adults who carry genetic or emotional risks may experience symptoms during periods of high pressure.
11. Is schizophrenia different from psychosis?
Yes. Psychosis is a symptom. Schizophrenia is a long-term condition that includes psychosis, thinking changes, emotional struggles, and social difficulties.
12. Can schizophrenia be mistaken for depression?
Absolutely. Both involve withdrawal, loss of interest, and emotional changes. Teens and adults often receive a depression label before deeper symptoms reveal the full picture.
13. Does schizophrenia look different across cultures?
Yes. Cultural beliefs shape how symptoms are interpreted. In India or the UAE, families may view early symptoms as stress or spiritual concerns. In the U.S. or UK, symptoms may be seen through a psychological lens. Culture affects help-seeking behavior, too.
14. What triggers schizophrenia in teenagers?
Teens may experience symptoms due to brain development, genetic factors, emotional stress, or substance use. These factors do not guarantee schizophrenia. They make the brain more sensitive during an already vulnerable stage.
15. Why do adults show more structured delusions?
Adults have mature thinking patterns. When symptoms appear, the ideas follow organized themes. This makes delusions more noticeable and easier to describe.
16. Can schizophrenia appear after trauma?
Trauma does not directly cause schizophrenia, but it can interact with vulnerability. Teens and adults may develop symptoms after emotionally overwhelming events. The trauma makes the brain more sensitive to stress.
17. How do schools usually react to early schizophrenia symptoms?
Schools often interpret symptoms as academic struggles, attention issues, or social difficulties. Teachers may not recognize the deeper patterns until the symptoms become disruptive.
18. Are adults more open about their symptoms than teens?
Many adults sense something is wrong and try to explain it. Teens, however, often hide their experiences because they fear judgment. Adults express their inner world more clearly, which helps with early recognition.
19. What should families look for if they suspect schizophrenia?
Watch for ongoing withdrawal, fear without clear reason, sudden loss of interest, unusual ideas, or noticeable thinking difficulties. Family members should trust their instincts if something feels off for a long time.
20. Do people with schizophrenia know something is wrong?
It varies. Many adults notice that their thoughts feel different. Teens may not realize anything unusual is happening. They may feel overwhelmed or confused but lack the language to explain it.
Final Closing Section
Schizophrenia is a complex condition, but understanding how symptoms differ between teenagers and adults brings clarity to families around the world. When the condition begins in adolescence, it hides behind ordinary teenage behavior, leaving families unsure of what they see. When it appears in adults, it disrupts routines, responsibilities, and relationships more visibly. These differences shape how symptoms are recognized, discussed, and supported.
Across the U.S., India, the UK, Australia, Canada, and the UAE, families share the same experience: uncertainty. They wonder if the changes are temporary or something deeper. They hesitate, hoping things will improve. They worry about what others will think. These emotions are universal. They show the weight people carry when they suspect something is changing in their loved one.
The key is to observe patterns rather than isolated moments. A teen who withdraws for a day may need rest. A teen who withdraws for weeks may need support. An adult who forgets one task is human. An adult who feels confused and overwhelmed for months may be facing something more complex. When families trust their instincts and pay attention to consistent changes, they recognize early signs sooner.
Knowledge reduces fear. Understanding reduces stigma. Compassion strengthens families. With awareness, teens and adults can navigate symptoms with dignity, clarity, and support. The journey becomes less frightening when families, friends, and communities respond with patience and understanding. Schizophrenia does not define a person. It is one part of a larger life, and with the right environment, many people continue to grow, connect, and find meaning beyond the symptoms.
About the Author
Srishty Bhadoria is a dedicated mental-health writer known for her clear, compassionate approach to complex psychological topics. Her work focuses on helping readers understand mental-health conditions in a practical, relatable way, while maintaining high standards of accuracy, depth, and empathy. With a strong interest in human behavior, emotional wellness, and the social factors that influence mental health across cultures, Srishty brings a global and inclusive perspective to her writing.
She has spent years studying how mental-health information is perceived by different age groups and how early awareness can shape outcomes for individuals and families. Srishty’s writing philosophy centers on bridging the gap between clinical knowledge and everyday understanding. She believes that mental-health education should be accessible, stigma-free, and grounded in real-life experiences.
Her goal as an author is to empower readers with knowledge they can trust. Whether discussing early signs of emotional distress, explaining complex disorders, or guiding families through difficult situations, Srishty strives to create content that supports, informs, and encourages meaningful conversations about mental health.
Transform Your Life with Expert Guidance from Click2Pro
At Click2Pro, we provide expert guidance to empower your long-term personal growth and resilience. Our certified psychologists and therapists address anxiety, depression, and relationship issues with personalized care. Trust Click2Pro for compassionate support and proven strategies to build a fulfilling and balanced life. Embrace better mental health and well-being with India's top psychologists. Start your journey to a healthier, happier you with Click2Pro's trusted online counselling and therapy services.






