Types of Bipolar Disorder: Distinguishing Between Bipolar I, II, and Cyclothymia
Table of Contents
- Why Misunderstanding Bipolar Disorder Is Dangerous in 2025
- Bipolar I Disorder: Beyond the Stereotype of “Just Mood Swings”
- Bipolar II Disorder: The Quiet Chaos of Hypomania and Depression
- Cyclothymia: The “Lesser Known Cousin” That’s Often Misunderstood
- Diagnostic Process: How Psychiatrists and Clinical Psychologists Differentiate the Three
- Bipolar vs Borderline Personality Disorder: Clearing the Confusion
- Treatment Strategies by Type (Not All Bipolar Disorders Are Treated the Same)
- Life With Bipolar: Long-Term Outlook, Relapse Prevention & Thriving
- Stigma and Shame in Indian Families: Why Early Intervention Is Critical
- When to Seek Help: Red Flags That Suggest It’s More Than a Mood Swing
- For Families & Friends: How to Support Without Overstepping
- Online Therapy and Diagnosis in India: Is It Reliable for Bipolar Disorders?
- FAQs
- About the Author
Why Misunderstanding Bipolar Disorder Is Dangerous in 2025
Mental health awareness may have grown in recent years, but when it comes to bipolar disorder, dangerous myths still thrive. Especially in 2025, where social media floods our screens with hashtags like mood swings or manic energy, the real weight of bipolar disorders gets lost in filters and reels.
In India, the misunderstanding goes a step further. Many still treat mood changes as either “stress-related,” a spiritual imbalance, or simply a phase. But bipolar disorder is none of these. It’s a chronic mental health condition that can disrupt every part of a person’s life—if not understood and managed early.
The real danger lies in mislabeling and underdiagnosing. A person with untreated bipolar disorder might live for years misdiagnosed as having depression or anxiety. In fact, it’s one of the most misdiagnosed conditions in clinical practice. The longer it remains unrecognized, the more severe and life-altering the episodes can become—impacting relationships, jobs, education, and even physical health.
Adding to the complexity is how bipolar symptoms often mirror everyday struggles: sadness, fatigue, excitement, irritability. But the intensity, frequency, and duration of these feelings are what set bipolar disorder apart. When a person’s low mood lasts for weeks or their energy becomes uncontrollably high for days, it’s no longer ordinary.
What makes it even more dangerous in 2025? The growing trend of self-diagnosis. People read a post, relate to a few signs, and conclude they have “bipolar.” But this often leads to either unnecessary panic or harmful dismissal. True diagnosis requires time, clinical evaluation, and a deeper look at one’s mental health history.
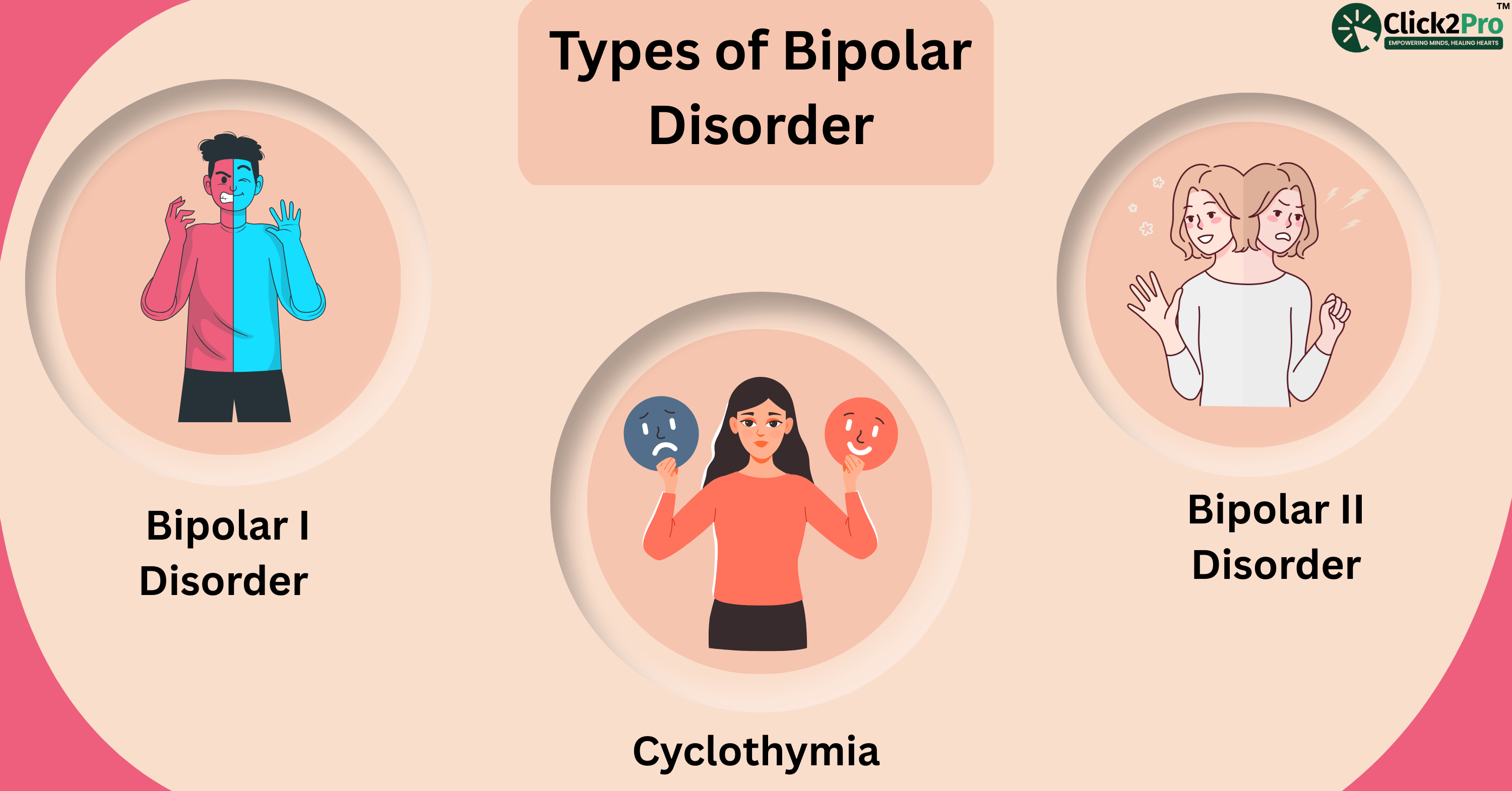
That’s why distinguishing between Bipolar I, Bipolar II, and Cyclothymia isn’t just a medical necessity—it’s a life-saving clarity.
Bipolar I Disorder: Beyond the Stereotype of “Just Mood Swings”
The term “bipolar” is often thrown around casually. Someone feels energized and creative one day, tired the next, and they say, “I must be bipolar.” But Bipolar I Disorder is not about daily ups and downs. It’s a serious condition where manic episodes can take over someone’s life and, at times, require hospitalization.
Let’s break this down in simple terms.
What makes Bipolar I stand out? The presence of full manic episodes—a state where the person feels extremely elevated or irritable for at least a week. This isn’t your average “good mood.” We’re talking about extreme confidence, racing thoughts, sleepless nights without fatigue, impulsive decisions, and sometimes even losing touch with reality.
These manic episodes can be so intense that the person may:
-
Quit their job suddenly.
-
Spend massive amounts of money impulsively.
-
Speak so rapidly that others can’t follow.
-
Believe they have special powers or are on a grand mission.
-
Engage in reckless sexual or social behavior without fear of consequences.
Often, these highs are followed by major depressive episodes—periods of deep sadness, guilt, loss of energy, and disconnection from the world. It’s this dramatic shift—from sky-high mania to crashing depression—that defines Bipolar I.
Now, here’s what many don’t realize: not all manic episodes feel euphoric. Some are agitated, angry, and paranoid. A person may seem aggressive, argue with loved ones, or feel like everyone is against them. This side of mania is rarely portrayed in films or social media, which contributes to misperceptions.
In India, such behavior is often misunderstood. Families may think the person is being stubborn, rebellious, or simply “acting out.” The lack of education around mental illness leads many people to spiritual healers or faith-based interventions first. While cultural beliefs play an important role in support systems, they should not replace clinical help when the signs are this severe.
Featured Snippet-Optimized Summary
What are the main symptoms of Bipolar I Disorder?
Bipolar I is defined by at least one manic episode lasting a week or requiring hospitalization. Symptoms include extreme energy, decreased need for sleep, risky behavior, inflated self-esteem, racing thoughts, and speech. Depressive episodes also occur, but one full manic episode is enough for diagnosis.
To understand Bipolar I is to recognize that it’s not about moods—it’s about mental states that can spiral dangerously if left unmanaged. Diagnosis is not about one “bad week” but a pattern observed over time. That's why a structured, compassionate, and informed approach is key.
Bipolar II Disorder: The Quiet Chaos of Hypomania and Depression
If Bipolar I is the loud storm, Bipolar II is the quiet thunder rumbling underneath. It often goes unnoticed, misjudged, or brushed off as regular emotional instability. But make no mistake—it’s equally serious and deeply disruptive.
Bipolar II Disorder is often misunderstood because it doesn’t involve full-blown mania. Instead, it includes something called hypomania—a milder, shorter-lived version of mania that can still cause harm. People with Bipolar II experience both hypomanic episodes and major depressive episodes, but never the full mania seen in Bipolar I.
So, what does hypomania look like? On the surface, a person may seem productive, enthusiastic, or even charming. They might speak more, sleep less, or feel unusually creative. That’s why people rarely see it as a problem. But beneath that surface, hypomania can impair judgment. Someone may overspend, take risky decisions, or push personal boundaries in ways that catch up later.
Then comes the crash—deep, long-lasting depression. This is what brings most people to therapy or counselling. The sadness lingers for weeks. There's a loss of interest in everything, trouble concentrating, feelings of guilt, and a heavy emotional numbness that’s difficult to explain to others. For many with Bipolar II, it’s the depression that rules their life, not the hypomania.
In India, especially among women, Bipolar II is often diagnosed late. The reason? Women are more likely to report sadness and fatigue rather than irritability or impulsivity. Hypomanic phases are often seen as “just being hyper” or “finally feeling good.” And because it doesn't disrupt daily life as obviously as mania does, family members often dismiss the signs.
What makes Bipolar II so difficult is this emotional pendulum—from energized and functional to drained and disconnected. It’s like having two conflicting realities within the same mind.
Featured Snippet-Optimized Summary
What is Bipolar II Disorder?
Bipolar II Disorder involves cycles of hypomania (a milder, elevated mood) and major depression. Unlike Bipolar I, it does not include full manic episodes but can still lead to significant life disruptions.
And here’s the irony: because hypomania can feel good or seem harmless, many people resist treatment. But without it, the depression returns harder, and the emotional swings become harder to control. Early diagnosis, observation of mood patterns, and open conversations are crucial.
Cyclothymia: The “Lesser Known Cousin” That’s Often Misunderstood
If Bipolar I is the high mountain and Bipolar II the steep valley, Cyclothymia is a long, winding road with unexpected curves. It’s subtle. It’s sneaky. And most importantly, it’s overlooked—even by mental health professionals.
Cyclothymia, or Cyclothymic Disorder, is marked by ongoing mood swings—mild highs and mild lows—that last for at least two years in adults. These highs aren’t quite hypomania, and the lows don’t qualify as full depression. But together, they form an unpredictable cycle that can deeply affect a person’s sense of self and stability.
What makes Cyclothymia especially tricky is that it often masquerades as personality traits. The person might seem moody, sensitive, inconsistent, or emotionally reactive. In school or the workplace, they may be seen as unreliable or dramatic. But in truth, they’re riding a constant wave of emotional fluctuations that they can’t fully control.
In India, Cyclothymia is rarely diagnosed on time. Many adolescents, especially, are misjudged as having behavioral issues. Families may describe them as “immature” or “too emotional.” Teachers may label them as inattentive or lazy. But no one connects the dots between their mood patterns and a deeper mental health concern.
What makes Cyclothymia dangerous is that it doesn’t always feel serious. A person might go months without major issues, only to suddenly experience weeks of instability. Because the emotional shifts are less intense, people delay seeking help until the patterns worsen—or develop into full-blown Bipolar I or II.
A common scenario might look like this: a person feels unusually energetic for a few days, starts multiple new activities, and then suddenly loses interest or becomes emotionally low for weeks. The pattern repeats over months or years. But without clinical observation, it remains “just a phase.”
Featured Snippet-Optimized Summary
What is Cyclothymia?
Cyclothymia is a mood disorder marked by fluctuating low-level depressive and hypomanic symptoms over two years. While not as intense as Bipolar I or II, it can develop into them if left untreated.
Diagnosing Cyclothymia requires patience and time. Psychologists often rely on mood diaries, therapy conversations, and family observations to identify the recurring pattern. It’s not about isolated emotions—it’s about sustained emotional rhythms that interfere with everyday functioning.
And yet, many people with Cyclothymia learn to mask their struggles. They adapt, they hide, they internalize. That’s why awareness is critical—not just for professionals, but for families, educators, and peers.
Diagnostic Process: How Psychiatrists and Clinical Psychologists Differentiate the Three
When someone shows symptoms of emotional highs and lows, it may seem simple to assume it’s bipolar disorder. But beneath the surface, accurate diagnosis requires much more than ticking off a symptom checklist. For professionals like psychiatrists and clinical psychologists, distinguishing between Bipolar I, Bipolar II, and Cyclothymia involves careful observation, repeated interviews, and contextual understanding of the person’s life and emotional history.
It starts with timing and pattern recognition. A full manic episode lasting at least seven days, or any manic behavior that leads to hospitalization, leans heavily toward Bipolar I. If the high-energy phases are shorter and milder, without hallucinations or severe disruption, yet followed by deep depression, Bipolar II becomes more likely.
In Cyclothymia, neither phase reaches diagnostic thresholds. Instead, the person experiences mild highs and lows continuously over at least two years. This makes it especially hard to catch, because symptoms don’t shout—they whisper.
Indian clinicians also have to take cultural context into account. For example, spiritual beliefs or family roles can sometimes blur the line between symptoms and social behavior. A young man speaking confidently about being chosen by a higher power may be perceived as religiously expressive—or he may be in a manic episode. It takes cultural sensitivity to interpret such signs correctly.
What professionals often use in therapy rooms is something called a “longitudinal clinical interview.” This means mapping out not just the current symptoms, but the person’s mood patterns, energy shifts, life changes, and functioning over months or even years. Tools like mood diaries, family interviews, and standardized scales may support this process.
It’s also important to rule out other conditions, such as substance-induced mood changes, personality disorders, or trauma-related emotional dysregulation.
Featured Snippet-Optimized Summary
How are Bipolar I, Bipolar II, and Cyclothymia diagnosed?
Diagnosis is based on the duration, intensity, and frequency of mood episodes. Bipolar I includes full mania, Bipolar II includes hypomania and depression, and Cyclothymia involves milder, long-term fluctuations. Clinical history and mood tracking are essential for accurate diagnosis.
Most importantly, a diagnosis is not a label—it’s a pathway to clarity. When done with empathy and expertise, it opens doors to support, self-awareness, and healing.
Bipolar vs Borderline Personality Disorder: Clearing the Confusion
One of the most commonly confused conditions in psychology today is the difference between bipolar disorder and borderline personality disorder (BPD). Both involve emotional instability. Both can cause impulsive decisions, mood shifts, and problems in relationships. But that’s where the similarity ends.
Think of it this way: Bipolar disorder is cyclical; BPD is moment-to-moment.
In bipolar disorder, emotional episodes happen in cycles—sometimes lasting days, weeks, or months. The mood swings are longer in duration and not always triggered by external events. For example, someone with Bipolar II may go through a full week of depression without any identifiable cause. In contrast, someone with BPD may feel abandoned or angry within minutes of a perceived slight or rejection.
Another key distinction is identity stability. People with BPD often struggle with a shifting sense of self. They may feel empty, not know who they are, or change their goals, values, and even personality traits often. This identity confusion is not typical in bipolar disorder, where the person usually has a more stable sense of who they are—just with emotional highs and lows.
Impulsivity also differs. In bipolar mania or hypomania, risky behavior often stems from elevated energy, overconfidence, or impaired judgment. But in BPD, impulsivity is usually tied to fear of abandonment or emotional pain. The driver is different, even if the action looks similar.
In India, this confusion is even more prevalent due to limited awareness about personality disorders. Many women, in particular, are misdiagnosed with bipolar disorder when they actually show traits of BPD. This mislabeling can lead to the wrong treatment approach and prolonged suffering.
Featured Snippet-Optimized Summary
What is the difference between Bipolar Disorder and Borderline Personality Disorder?
Bipolar disorder involves long-term mood episodes like mania or depression, while BPD involves rapid, situation-triggered mood changes, identity instability, and fear of abandonment. Timing, triggers, and emotional duration help distinguish the two.
Proper diagnosis is critical because treatment strategies are different. Bipolar disorder often requires mood stabilizers, while BPD responds better to specialized therapy like DBT (Dialectical Behavior Therapy). Misdiagnosis can delay effective healing and increase emotional distress.
Recognizing these subtle yet significant differences ensures that people receive the care they truly need—not just a label, but a real understanding of what they’re going through.
Treatment Strategies by Type (Not All Bipolar Disorders Are Treated the Same)
One of the biggest misconceptions about bipolar disorder is that there's a one-size-fits-all treatment. In reality, the approach varies depending on the type—Bipolar I, Bipolar II, or Cyclothymia. Each has different needs, risks, and treatment responses. Understanding this difference can mean the difference between ongoing struggles and long-term stability.
Bipolar I: Managing Full Mania and Deep Depression
In Bipolar I, the emotional highs and lows can be intense and deeply disruptive. Managing this condition begins with understanding the patterns behind these episodes. It’s not just about responding when things get out of control—it’s about building systems that prevent those extremes from returning.
Psychotherapy plays a critical role in this process. Sessions help individuals recognize their personal triggers, develop strategies to manage intense emotional shifts, and stay consistent with routines that promote stability.
Therapists often focus on emotional regulation, sleep hygiene, and communication strategies to prevent interpersonal conflicts that may arise during manic or depressive periods. Over time, individuals learn how to monitor their moods, respond early to red flags, and ask for support when needed.
Even though Bipolar I can involve severe episodes, many people regain control of their lives through structured care, lifestyle consistency, and a supportive mental health team.
Bipolar II: Targeting Depression and Preventing Escalation
People with Bipolar II often experience more time in depression than in hypomania. Because of this, therapy becomes the cornerstone of long-term management. One of the most helpful approaches is Cognitive Behavioral Therapy (CBT), which helps individuals identify and shift negative thought patterns that contribute to depressive episodes.
Therapists also work on strength-building techniques, like setting realistic goals, practicing mindfulness, and improving self-esteem. Since emotional changes in Bipolar II can feel subtle at first, therapy provides a safe space to explore these shifts before they escalate.
Managing Bipolar II isn’t about eliminating all mood changes. It’s about gaining insight, learning how to respond to internal changes, and creating a resilient emotional routine. When practiced consistently, these strategies help reduce relapses and give individuals greater control over their daily lives.
Lifestyle adjustments also form a strong foundation here. Maintaining a regular sleep schedule, avoiding alcohol or stimulants, and tracking mood changes daily help reduce relapse risk.
Cyclothymia: Focused on Patterns, Not Just Symptoms
Treating Cyclothymia is less about prescriptions and more about long-term emotional regulation. Many people with Cyclothymia experience mood shifts that aren’t extreme—but they are persistent and disruptive if left unaddressed.
The most effective path forward often includes therapy, journaling, and structured daily habits. These tools help individuals understand their mood patterns and gain clarity on what triggers their emotional highs and lows.
A therapist may assist in identifying early warning signs, teaching coping strategies, and supporting long-term emotional balance. Since mood changes in Cyclothymia are subtle but chronic, the key lies in early recognition and consistent mental health support.
Building a steady lifestyle—getting enough sleep, maintaining routines, managing stress—can make a noticeable difference. The goal is to create emotional stability, even if the fluctuations never fully disappear.
Featured Snippet-Optimized Summary
Do different types of bipolar disorder require different treatments?
Yes. Bipolar I typically involves managing intense mood episodes. Bipolar II focuses more on regulating depression and emotional patterns. Cyclothymia relies on therapy, self-awareness, and lifestyle changes.
Regardless of type, consistency in care and emotional monitoring is essential. Progress comes from sustained support, not from reacting only during crises.
Life With Bipolar: Long-Term Outlook, Relapse Prevention & Thriving
A bipolar diagnosis doesn’t mean life stops. In fact, with proper treatment and self-awareness, many people live deeply meaningful, productive lives. But stability doesn't come overnight—it comes through understanding, structure, and support.
Managing Daily Life: Structure Is Key
People living with bipolar disorder thrive on routine. That’s not just advice—it’s science. Regular sleep, consistent meal times, and scheduled downtime help stabilize mood cycles. Skipping sleep, for instance, is one of the most common triggers for manic or hypomanic episodes.
Mood tracking—whether with journals or apps—is another powerful tool. It helps individuals notice patterns, spot early signs of an oncoming episode, and take action before things escalate.
Some find comfort in meditation, yoga, or creative activities. These don’t cure bipolar disorder, but they help reduce anxiety, provide emotional outlets, and build self-awareness.
Relapse Prevention: Know the Red Flags
Relapse can happen, but it’s often preventable with the right signals in place. Some early signs include:
-
Sleeping less but feeling overly energetic
-
Becoming irritable without reason
-
Racing thoughts or speech
-
Withdrawal from social life
-
Sudden loss of interest in things once enjoyed
Having a plan in place—one that involves a trusted friend, partner, or therapist—can help catch these signs before they escalate. Many people prepare Relapse Action Plans, which include emergency contacts, self-care routines, and emotional grounding techniques to stay on track during challenging times.
The Power of Support and Self-Belief
In Indian society, where emotional issues are often hidden, open conversations about bipolar disorder are still rare. But that’s changing. More people are sharing their stories, asking for help, and breaking the stigma. Support groups, online platforms, and professional therapy are now more accessible than ever.
Living with bipolar disorder doesn’t mean you’ll always struggle. It means you may need to work a bit harder on balance. But in that effort, many people discover a deeper strength, sharper creativity, and more meaningful relationships than they ever imagined.
Featured Snippet-Optimized Summary
Can people with bipolar disorder live normal lives?
Yes. With regular treatment, self-care routines, support systems, and relapse planning, people with bipolar disorder can lead fulfilling, stable, and successful lives.
Stigma and Shame in Indian Families: Why Early Intervention Is Critical
Mental health stigma is a global challenge—but in many Indian households, it carries a heavy weight of silence, shame, and misunderstanding. When it comes to bipolar disorder, the issue deepens. The highs are dismissed as “drama,” the lows as “weakness,” and therapy as something for the “mentally unstable.” This cultural mindset prevents early help—and that delay can cost lives.
In Indian families, emotional concerns are often seen as private matters to be dealt with quietly. If a family member shows signs of extreme energy or sadness, they’re more likely to be scolded or advised to “be stronger” rather than taken to a psychologist. Manic behavior may be seen as rebellious, and depressive symptoms as laziness or a lack of faith. These beliefs don’t come from cruelty—they come from a lack of awareness passed down for generations.
Early intervention in bipolar disorder is vital. The longer symptoms go untreated, the more intense and unpredictable the episodes can become. Studies show that early diagnosis and consistent support greatly reduce the risk of hospitalization, suicide attempts, and long-term disability. Yet in many Indian homes, the fear of being labeled “paagal” keeps families from reaching out.
This delay also places emotional stress on the person affected. They start questioning themselves, suppressing feelings, and blaming their character. Over time, this can lead to dangerous isolation, especially among teenagers and young adults who often go unnoticed.
The solution lies in conversations. Families need psychoeducation—not lectures, but honest, empathetic talks about what bipolar disorder really is. Early signs, mood tracking, and supportive therapy sessions should become part of household awareness, not taboo topics.
Featured Snippet-Optimized Summary
Why is early intervention important in bipolar disorder in India?
Due to stigma in Indian families, many bipolar symptoms are misunderstood or ignored. Early diagnosis prevents severe episodes, reduces long-term risk, and improves recovery outcomes.
Breaking the silence isn’t easy, but it’s essential. When families shift from blame to understanding, from shame to support, healing truly begins.
When to Seek Help: Red Flags That Suggest It’s More Than a Mood Swing
Everyone has emotional ups and downs. But how do you know when it crosses the line into something deeper, like bipolar disorder? This is one of the most common questions asked by people unsure about their own mental health or that of a loved one.
The key is pattern, intensity, and duration.
Here are some red flags that suggest a person might need professional evaluation—not just rest or motivation:
-
Mood episodes that last several days or more, either very low or extremely high.
-
Sudden changes in energy—from barely being able to move to feeling invincible overnight.
-
Irrational decisions, like quitting a job impulsively or spending large sums of money recklessly.
-
Trouble sleeping, especially a decreased need for sleep without feeling tired.
-
Unusual speech patterns, such as talking rapidly, jumping between ideas, or becoming difficult to interrupt.
-
Paranoia or delusions, particularly in manic states.
-
Feeling detached from reality, confused, or emotionally disconnected.
-
Long periods of hopelessness, especially if paired with suicidal thoughts or withdrawal from life.
If these symptoms repeat or form a noticeable pattern, it’s time to consult a psychologist or psychiatrist.
In India, many wait until a crisis before seeking help—such as a failed exam, relationship breakdown, or public outburst. But mental health doesn’t need a breaking point. Early consultation can clarify whether it’s stress, anxiety, or a bipolar pattern.
Even parents, partners, and friends should be mindful. If someone around you changes drastically—sleep patterns, speech, motivation, or risk-taking behavior—don’t hesitate to suggest a professional conversation. The sooner a pattern is recognized, the easier it is to manage and support.
Featured Snippet-Optimized Summary
When should someone with mood swings seek help?
If emotional highs or lows last several days, disrupt daily life, or include impulsivity, delusions, or disconnection from reality, it's time to consult a mental health professional.
Seeking help is not a weakness—it’s a strength. And catching bipolar disorder early gives individuals and families the best chance at understanding, healing, and thriving together.
For Families & Friends: How to Support Without Overstepping
Support from family and friends plays a huge role in managing bipolar disorder—but it’s a delicate balance. Too much involvement can feel invasive. Too little can feel like neglect. The key is knowing how to show up without controlling the journey.
In Indian households, loved ones often take charge—sometimes out of care, sometimes out of fear. Parents may insist on treatment paths without listening. Partners may misinterpret symptoms as moodiness or personal attacks. Friends might withdraw out of confusion. But bipolar disorder is not a character flaw—it’s a medical condition. And the way loved ones respond can either heal or harm.
The first step is learning. Take time to understand what bipolar disorder really is: its types, triggers, and how it affects thinking, emotions, and behavior. This removes blame and replaces it with compassion.
Second, listen more than you speak. Instead of pushing someone to “get better soon” or offering advice, simply say, “I’m here. Tell me how I can help.” This shows respect and avoids adding pressure during an episode.
Third, help with structure, not control. Offer reminders about appointments or help build routines around sleep, meals, or exercise. But avoid treating the person like a child or patient—maintain dignity and equality.
Importantly, set healthy boundaries. Supporting someone doesn’t mean sacrificing your own well-being. It’s okay to step back when overwhelmed and encourage professional intervention.
Lastly, celebrate small wins. A full day of work, a therapy breakthrough, or even maintaining routine for a week—these moments matter. Acknowledge them. They build hope.
Featured Snippet-Optimized Summary
How can families support someone with bipolar disorder?
By learning about the condition, listening empathetically, offering structured support, respecting boundaries, and encouraging treatment, families can be a vital part of recovery without overstepping.
Support doesn’t mean fixing someone. It means walking beside them with patience, not pushing from behind.
Online Therapy and Diagnosis in India: Is It Reliable for Bipolar Disorders?
India’s mental health landscape is evolving. With therapy becoming more accessible online, many individuals now turn to apps or digital platforms to seek help—especially for complex conditions like bipolar disorder. But a question arises: Is online therapy India reliable for diagnosing and managing bipolar disorders?
The short answer is: Yes—with some important conditions.
For milder symptoms, mood tracking, psychoeducation, and regular check-ins, online therapy can be highly effective. Video sessions with trained psychologists offer privacy, convenience, and affordability. For those living in tier-2 or tier-3 cities with limited access to mental health clinics, online options can be a lifeline.
However, bipolar disorder—especially Bipolar I—requires clinical observation over time. Severe symptoms like mania or psychosis may not always be evident in one call or session. That’s why diagnosis is often more reliable when the therapist has a long-term engagement with the client, supported by mood logs, family insights, and consistent tracking.
Also, not every online platform is equipped for such complexity. It’s important that therapists are qualified, experienced, and follow ethical standards. Look for platforms that offer continuity of care, allow feedback, and provide referral options if the case requires psychiatric intervention.
Online therapy also benefits from digital tools like mood tracking apps, journaling prompts, and goal setting frameworks, which help individuals stay engaged between sessions. These features make therapy more dynamic and self-driven, especially for Bipolar II and Cyclothymia.
Ultimately, blending online therapy with offline support, such as regular check-ins or in-person consultations, often offers the best of both worlds. The goal is not just diagnosis—it’s about long-term emotional care, consistent engagement, and timely intervention when needed.
By combining professional guidance with personal commitment, individuals can build a sustainable path toward mental wellness—no matter where they start.
Featured Snippet-Optimized Summary
Is online therapy reliable for bipolar disorder in India?
Online therapy can be effective for managing and identifying bipolar symptoms, especially in early stages or milder forms. Long-term observation, consistent engagement, and clinical oversight are key for accuracy and support.
For Indian users who face stigma or time constraints, online therapy offers a discreet, flexible path to healing. But make sure it’s with the right professionals—and part of a long-term care plan.
FAQs
1. What is the main difference between Bipolar I and Bipolar II?
The key difference lies in the type of "high" experienced. Bipolar I involves full manic episodes, which can include extreme energy, risky behavior, and sometimes psychosis. Bipolar II involves hypomania, which is milder but still disruptive, followed by longer and deeper periods of depression.
2. Is Cyclothymia a form of bipolar disorder?
Yes. Cyclothymia is considered a milder, chronic form of bipolar disorder. It involves ongoing mood swings—emotional highs and lows—that don’t meet the full criteria for mania or major depression. However, if untreated, it can develop into Bipolar I or II over time.
3. Can bipolar disorder be mistaken for depression or anxiety?
Absolutely. Many people with Bipolar II or Cyclothymia are first diagnosed with depression or anxiety because their hypomanic symptoms are subtle or overlooked. This is why tracking mood patterns and seeking professional diagnosis is important.
4. Can someone live a normal life with bipolar disorder?
Yes. With the right treatment, self-care routine, and support system, many people with bipolar disorder lead stable, fulfilling lives. Consistency in therapy, medication (if required), and understanding one’s emotional patterns are key.
5. How long do bipolar episodes last?
It varies by type. A manic episode in Bipolar I can last a week or more, while depressive episodes can last several weeks to months. In Bipolar II, hypomania may last a few days, followed by longer depression. Cyclothymia involves milder symptoms lasting over two years.
6. What are the early warning signs of bipolar disorder?
Early signs may include dramatic mood changes, reduced need for sleep, talking quickly, impulsive decisions, or feeling overly energized or low without reason. When such patterns repeat or disrupt daily life, it’s time to seek professional help.
7. Can bipolar disorder be diagnosed through online therapy in India?
Yes, online therapy can help with diagnosis and management, especially in early or moderate cases. Platforms that provide licensed therapists and ongoing support can be effective. However, for severe symptoms like psychosis, in-person evaluation may be required for accuracy.
About the Author
Naincy Priya is a seasoned Clinical Psychologist (Associate) with over 11 years of experience in the mental health field. She holds a Ph.D. in Psychology and is currently affiliated with Click2Pro, where she serves as a Senior Psychologist. Her expertise encompasses a wide range of mental health issues, including anxiety, depression, obsessive-compulsive disorder (OCD), and relationship counselling.
Dr. Priya is proficient in various therapeutic modalities such as Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), Acceptance and Commitment Therapy (ACT), Narrative Therapy, Motivational Enhancement Therapy (MET), Eye Movement Desensitization and Reprocessing (EMDR) Therapy, and Family and Marital Therapy. She adopts a holistic approach to patient care, considering the psychosocial elements influencing mental health and striving to understand each individual's unique context.
In her practice, Dr. Priya creates a non-judgmental environment, enabling clients to explore their cognitive processes, thought patterns, and behaviors. Her goal is to empower individuals to navigate their emotions and cultivate a wholesome existence that champions mental well-being and an enriched quality of life.
Beyond her clinical work, Dr. Priya is dedicated to raising awareness about mental health issues, particularly in the Indian context, where stigma often hinders early intervention. She emphasizes the importance of early diagnosis and consistent support to reduce the risk of hospitalization, suicide attempts, and long-term disability associated with untreated mental health conditions.
Her commitment to mental health advocacy and her extensive experience make her a valuable resource for individuals seeking guidance and support in their mental health journey.
Transform Your Life with Expert Guidance from Click2Pro
At Click2Pro, we provide expert guidance to empower your long-term personal growth and resilience. Our certified psychologists and therapists address anxiety, depression, and relationship issues with personalized care. Trust Click2Pro for compassionate support and proven strategies to build a fulfilling and balanced life. Embrace better mental health and well-being with India's top psychologists. Start your journey to a healthier, happier you with Click2Pro's trusted online counselling and therapy services.






