The Connection Between Body Dysmorphic Disorder and Eating Disorders
Table of Contents
- Comorbidity Between BDD and Eating Disorders
- Prevalence and Demographics
- Comorbidity Between Body Dysmorphic Disorder (BDD) and Eating Disorders
- Shared Psychological Factors Between Body Dysmorphic Disorder and Eating Disorders
- Neurological and Biological Underpinnings of Body Dysmorphic Disorder and Eating Disorders
- Sociocultural Influences on Body Dysmorphic Disorder and Eating Disorders
- Diagnostic Challenges in Co-occurring Body Dysmorphic Disorder and Eating Disorders
- Treatment Approaches for Co-occurring Body Dysmorphic Disorder and Eating Disorders
- Case Studies and Testimonials
- Resources and Support Systems for Body Dysmorphic Disorder and Eating Disorders in India
- Conclusion
- FAQs
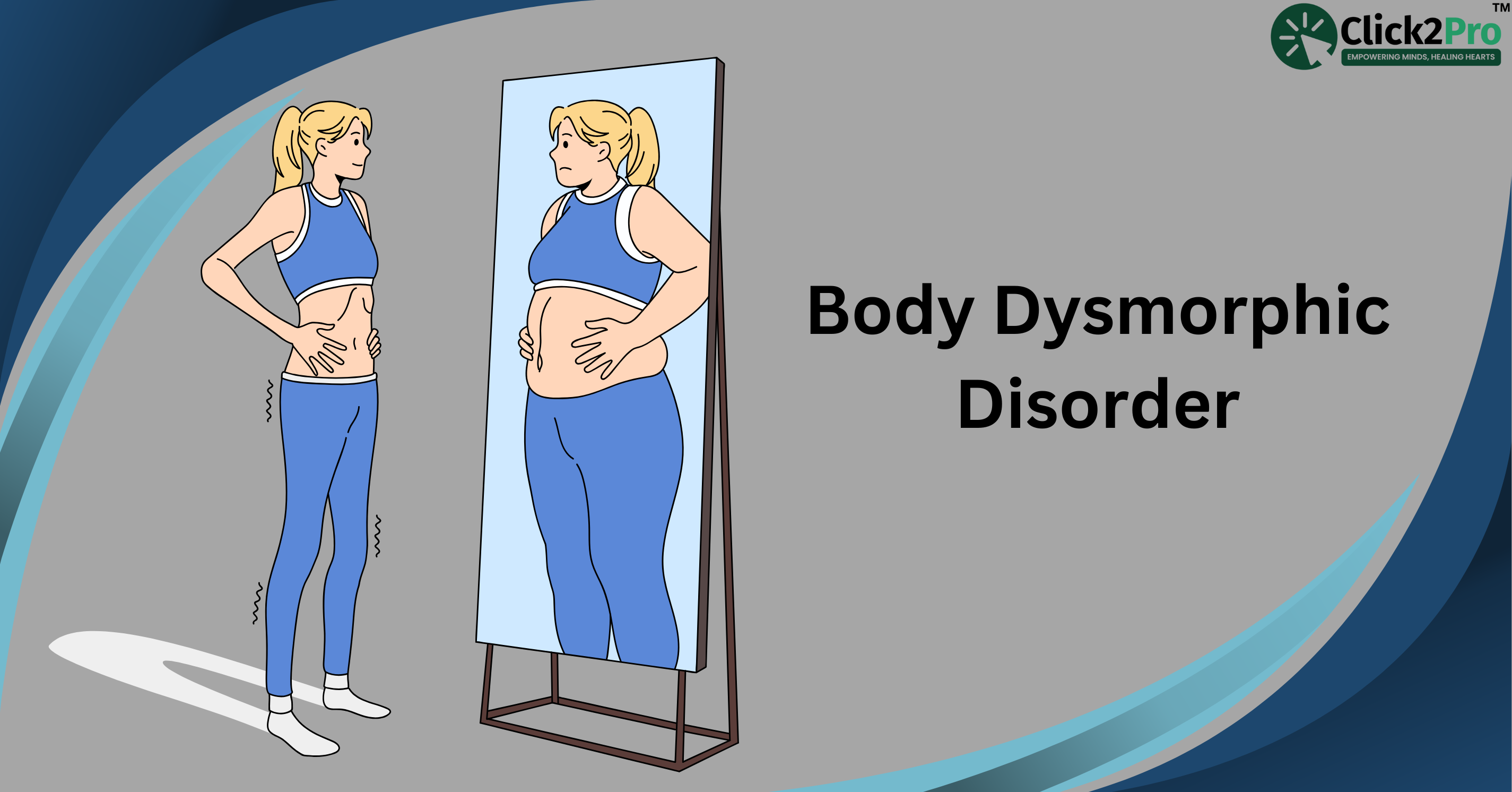
Body Dysmorphic Disorder (BDD) and eating disorders are significant mental health concerns affecting individuals worldwide, including a notable presence in India. BDD involves an obsessive focus on perceived flaws in one's appearance, leading to distress and impaired daily functioning. Eating disorders, such as anorexia nervosa and bulimia nervosa, encompass unhealthy relationships with food and body image, often resulting in severe physical and psychological consequences. Understanding the connection between body dysmorphia and eating disorders is crucial for effective diagnosis and treatment.
Prevalence and Impact
The prevalence of BDD varies globally, with studies indicating that approximately 1.7% to 2.9% of the general population is affected. In India, research focusing on body image dissatisfaction (BID) in rural areas highlights the pervasive nature of these concerns across diverse age groups. Traditional beauty standards, cultural practices, and limited access to mental health resources contribute to the manifestation of BID, which can be a precursor to both BDD and eating disorders.
Eating disorders in India exhibit a wide prevalence range, from 4% to 45.4%, influenced by factors such as urbanization, cultural transitions, and societal pressures. Medical students, in particular, have shown a higher vulnerability, with a meta-analysis revealing a prevalence rate of 10.4% among this group.
Comorbidity Between BDD and Eating Disorders
A significant overlap exists between body dysmorphic disorder and eating disorders. Research indicates that 32.5% of individuals diagnosed with BDD also experience a comorbid eating disorder. This comorbidity includes 9.0% with anorexia nervosa, 6.5% with bulimia nervosa, and 17.5% with other specified eating disorders.
Table: Comorbidity of BDD and Eating Disorders
|
Comorbid Condition |
Percentage |
|
Anorexia Nervosa |
9.0% |
|
Bulimia Nervosa |
6.5% |
|
Other Specified Eating Disorders |
17.5% |
Understanding the Connection
The intricate relationship between body dysmorphia and eating disorders can be attributed to shared psychological factors, including body image disturbance, perfectionism, and low self-esteem. Individuals with BDD often exhibit an intense preoccupation with perceived physical defects, which can lead to disordered eating behaviors as a means to 'correct' or control these flaws. Conversely, those with eating disorders may develop obsessive concerns about specific body parts, aligning with characteristics of BDD.
Cultural and societal influences play a pivotal role in the development and perpetuation of both disorders. In the Indian context, traditional beauty ideals, combined with the increasing impact of global media, contribute to heightened body dissatisfaction. This dissatisfaction can manifest as either body dysmorphia, eating disorders, or a combination of both.
Prevalence and Demographics
Understanding the prevalence and demographics of Body Dysmorphic Disorder (BDD) and eating disorders is essential for developing effective public health strategies and interventions. These conditions affect diverse populations worldwide, with varying rates influenced by cultural, societal, and economic factors.
Body Dysmorphic Disorder (BDD):
-
Prevalence: BDD affects approximately 1.7% to 2.9% of the global population.
-
Gender Distribution: Studies indicate that BDD impacts about 2.5% of women and 2.2% of men in the United States, suggesting a slightly higher prevalence among females.
-
Age of Onset: BDD often manifests during adolescence, with a significant number of cases developing before the age of 18.
Eating Disorders:
-
Prevalence: Eating disorders, including anorexia nervosa, bulimia nervosa, and binge eating disorder, affect up to 5% of the population in the United States.
-
Gender Distribution: These disorders are more prevalent in females, with anorexia affecting approximately 0.4% of young women annually and bulimia about 1.3%. Binge eating disorder shows a prevalence of 1.6% among women and 0.8% among men.
-
Age of Onset: Eating disorders typically emerge during adolescence or early adulthood, though they can develop at any age.
Indian Context
Body Dysmorphic Disorder (BDD):
-
Prevalence: While specific nationwide prevalence data for BDD in India is limited, studies focusing on body image dissatisfaction (BID) in rural areas reveal a significant concern across diverse age groups. Traditional beauty standards, cultural practices, and limited access to mental health resources contribute to the manifestation of BID, which can be a precursor to BDD.
Eating Disorders:
-
Prevalence: In India, the prevalence of eating disorders ranges from 4% to 45.4%, with higher rates observed in urban areas. This wide range reflects the influence of urbanization, cultural transitions, and societal pressures.
-
Gender Distribution: Eating disorders are more common among females, but increasing cases among males have been reported, particularly related to muscle dysmorphia.
-
Age of Onset: These disorders often begin in adolescence or early adulthood, with studies indicating a higher vulnerability among medical students, showing a prevalence rate of 10.4% in this group.
Implications
The data underscores the pressing need for awareness, early diagnosis, and intervention strategies tailored to diverse populations. In India, the significant prevalence of eating disorders and the cultural factors contributing to body image dissatisfaction highlight the necessity for culturally sensitive mental health services. Addressing these issues requires a multifaceted approach, including public education, accessible treatment options, and ongoing research to inform policy and practice.
Comorbidity Between Body Dysmorphic Disorder (BDD) and Eating Disorders
Body Dysmorphic Disorder (BDD) and eating disorders are distinct mental health conditions; however, they frequently co-occur, leading to complex clinical presentations. Understanding the extent and nature of this comorbidity is crucial for effective diagnosis and treatment.
Clinical Implications
The coexistence of BDD and eating disorders presents unique challenges in clinical settings. Individuals with both conditions often exhibit more severe psychopathology and body image disturbances compared to those with either disorder alone. This comorbidity is associated with higher rates of psychiatric hospitalizations and increased utilization of mental health services. Moreover, the presence of both disorders can complicate treatment, necessitating integrated therapeutic approaches that address the full spectrum of symptoms.
Gender Differences
Studies have shown that females with BDD are more likely to have a comorbid eating disorder than males. This gender disparity may be influenced by societal and cultural pressures emphasizing thinness and appearance ideals for women. However, it's important to note that males with BDD can also experience significant body image concerns, often related to muscularity, which may lead to disordered eating behaviors aimed at increasing muscle mass.
Age of Onset
Both BDD and eating disorders commonly manifest during adolescence or early adulthood. The early onset of these disorders underscores the importance of early detection and intervention. Adolescents with comorbid BDD and eating disorders may face compounded challenges, including heightened body dissatisfaction and a greater risk of developing chronic mental health issues if not addressed promptly.
Shared Psychopathological Features
The comorbidity between BDD and eating disorders may be attributed to shared psychopathological features, such as:
-
Body Image Disturbance: Both disorders involve a distorted perception of one's body, leading to significant distress and impairment.
-
Perfectionism: Individuals often exhibit high levels of perfectionism, striving for an unattainable body ideal.
-
Obsessive-Compulsive Traits: Repetitive behaviors and intrusive thoughts related to appearance are common in both conditions.
Treatment Considerations
Addressing comorbid BDD and eating disorders requires a comprehensive and multidisciplinary approach:
-
Integrated Therapy: Combining cognitive-behavioral therapy (CBT) techniques tailored to both BDD and eating disorders can be effective.
-
Pharmacotherapy: Selective serotonin reuptake inhibitors (SSRIs) may help alleviate symptoms of both disorders.
-
Nutritional counselling: Guidance from dietitians can assist in establishing healthy eating patterns and addressing nutritional deficiencies.
-
Family Involvement: Family-based interventions can provide support and improve treatment adherence, especially in adolescents.
The significant comorbidity between Body Dysmorphic Disorder and eating disorders highlights the need for heightened clinical awareness and integrated treatment strategies. By addressing the intertwined nature of these conditions, healthcare providers can improve outcomes and enhance the quality of life for affected individuals.
Shared Psychological Factors Between Body Dysmorphic Disorder and Eating Disorders
Body Dysmorphic Disorder (BDD) and eating disorders are complex mental health conditions that often coexist, sharing several psychological factors that contribute to their development and persistence. Understanding these shared factors is crucial for effective diagnosis and treatment.
Body Image Disturbance
A central feature of both BDD and eating disorders is body image disturbance. Individuals with these conditions experience a distorted perception of their physical appearance, leading to significant emotional distress and maladaptive behaviors aimed at altering their bodies. This misperception often results in obsessive thoughts and compulsive actions related to appearance and body weight.
Perfectionism
Perfectionism is another common trait observed in individuals with BDD and eating disorders. The relentless pursuit of an unattainable ideal can result in obsessive thoughts and compulsive actions related to appearance and body weight. This perfectionistic tendency often intertwines with low self-esteem, where individuals base their self-worth predominantly on their physical appearance. Such a narrow self-evaluation can exacerbate feelings of inadequacy and perpetuate the cycle of negative body image and disordered eating behaviors.
Anxiety and Depression
Both BDD and eating disorders are associated with high levels of anxiety and depression. The preoccupation with perceived flaws or body weight can lead to social withdrawal, heightened self-consciousness, and a persistent state of distress. These emotional challenges further entrench individuals in their maladaptive behaviors, making recovery more complex.
Obsessive-Compulsive Traits
Individuals with BDD and eating disorders often exhibit obsessive-compulsive traits. These may manifest as repetitive behaviors such as mirror checking, excessive grooming, or ritualistic eating patterns. The compulsions serve as attempts to alleviate anxiety related to body image but often reinforce the obsessive thoughts, creating a vicious cycle.
Low self-esteem is prevalent among those with BDD and eating disorders. Individuals may base their self-worth predominantly on their physical appearance, leading to feelings of inadequacy and self-criticism. This diminished self-esteem can drive the pursuit of perfectionism and exacerbate body image disturbances.
Emotional Dysregulation
Emotional dysregulation, or difficulty managing and responding to emotional experiences, is another shared factor. Individuals may use disordered eating behaviors or appearance-focused rituals as coping mechanisms to manage negative emotions, which can perpetuate the disorders.
Social and Cultural Influences
Societal and cultural pressures play a significant role in both BDD and eating disorders. The portrayal of idealized body types in media and social platforms can contribute to body dissatisfaction and the internalization of unrealistic appearance standards. This external pressure can exacerbate existing vulnerabilities related to body image.
Table: Shared Psychological Factors Between BDD and Eating Disorders
|
Psychological Factor |
Description |
|
Body Image Disturbance |
Distorted perception of physical appearance leading to distress and maladaptive behaviors. |
|
Perfectionism |
Relentless pursuit of unattainable ideals, resulting in obsessive thoughts and compulsive actions. |
|
Anxiety and Depression |
High levels of anxiety and depression associated with preoccupation over perceived flaws. |
|
Obsessive-Compulsive Traits |
Repetitive behaviors aimed at alleviating appearance-related anxiety. |
|
Low Self-Esteem |
Self-worth predominantly based on physical appearance, leading to feelings of inadequacy. |
|
Emotional Dysregulation |
Difficulty managing emotions, leading to reliance on maladaptive coping mechanisms. |
|
Social and Cultural Influences |
External pressures from societal standards contributing to body dissatisfaction. |
Interaction of Shared Psychological Factors in BDD and Eating Disorders
Implications for Treatment
Understanding these shared psychological factors is crucial for developing integrated therapeutic approaches. Treatment plans should address body image disturbances, perfectionism, and associated emotional distress. Cognitive-behavioral therapy (CBT) has been effective in targeting these areas, helping individuals reframe distorted thoughts and develop healthier behaviors. Additionally, incorporating strategies to enhance emotional regulation and self-esteem can be beneficial. Given the influence of social and cultural factors, psychoeducation and media literacy can also play a role in mitigating external pressures.
The overlap of psychological factors in BDD and eating disorders necessitates a comprehensive and multifaceted treatment approach. By addressing the underlying shared factors, clinicians can better support individuals on their path to recovery.
Neurological and Biological Underpinnings of Body Dysmorphic Disorder and Eating Disorders
Body Dysmorphic Disorder (BDD) and eating disorders, such as anorexia nervosa and bulimia nervosa, are complex psychiatric conditions characterized by severe disturbances in body image and associated behaviors. Emerging research has begun to elucidate the neurological and biological underpinnings that may link these disorders, providing insights into their development and maintenance.
Neurobiological Factors
- Brain Structure and Function:
Visual Processing Abnormalities: Individuals with BDD and eating disorders often exhibit dysfunctions in brain regions responsible for visual and emotional processing. Studies have identified abnormalities in the frontostriatal and limbic systems, which may contribute to the obsessive thoughts and compulsive behaviors observed in both disorders.
- Neurotransmitter Systems:
Serotonin Dysregulation: Alterations in serotonin levels have been implicated in both BDD and eating disorders. Serotonin plays a crucial role in mood regulation, impulse control, and appetite, and its dysregulation may contribute to the anxiety, obsessive thoughts, and disordered eating behaviors characteristic of these conditions.
Dopaminergic Pathways: Dopamine, associated with reward processing and motivation, has also been linked to eating disorders. Dysfunction in dopaminergic pathways may influence binge-eating behaviors and the compulsive nature of certain eating disorders.
Genetic Factors
- Heritability:
Familial Aggregation: Research indicates a significant genetic component in the susceptibility to both BDD and eating disorders. Family studies have shown that first-degree relatives of individuals with these disorders have a higher likelihood of developing similar conditions, suggesting a hereditary predisposition.
- Genetic Associations:
Genome-Wide Association Studies (GWAS): Recent GWAS have identified specific genetic loci associated with eating disorders, providing insights into their complex genetic architecture. These studies highlight the interplay between genetic factors and environmental influences in the manifestation of these disorders.
Hormonal Influences
- Endocrine Factors:
Hormonal Dysregulation: Hormonal changes, particularly during critical developmental periods such as adolescence, may influence the onset and progression of BDD and eating disorders. Fluctuations in hormones like estrogen and cortisol have been studied for their potential roles in modulating mood, stress responses, and body image perceptions.
Implications for Treatment
Understanding the neurological and biological underpinnings of BDD and eating disorders is essential for developing targeted and effective treatments. Interventions may include:
-
Pharmacotherapy: Medications that modulate neurotransmitter systems, such as selective serotonin reuptake inhibitors (SSRIs), have shown efficacy in reducing symptoms of both BDD and certain eating disorders.
-
Neuromodulation Techniques: Emerging treatments like transcranial magnetic stimulation (TMS) are being explored for their potential to alter dysfunctional brain activity patterns associated with these disorders.
-
Integrated Therapeutic Approaches: Combining pharmacological treatments with psychotherapeutic interventions, such as cognitive-behavioral therapy (CBT), may address both the biological and psychological aspects of these conditions, leading to more comprehensive and sustained recovery outcomes.
The convergence of neurological and biological research has significantly advanced our understanding of Body Dysmorphic Disorder and eating disorders. By elucidating the complex interplay of brain function, genetic predispositions, and hormonal influences, this body of knowledge paves the way for more nuanced and effective treatment strategies, offering hope to those affected by these challenging conditions.
Sociocultural Influences on Body Dysmorphic Disorder and Eating Disorders
Body Dysmorphic Disorder (BDD) and eating disorders are complex mental health conditions significantly influenced by sociocultural factors. Understanding these influences is crucial for developing effective prevention and intervention strategies.
Media and Beauty Standards
The portrayal of idealized body types in media profoundly impacts individuals' perceptions of their own bodies. Social media platforms, in particular, inundate users with images and messages promoting unattainable beauty standards. This constant exposure can lead to body dysmorphia, as individuals compare themselves to curated and often digitally altered representations. Studies have linked increased social media usage to the development of body dysmorphic disorder and eating disorders, highlighting the role of these platforms in normalizing specific beauty criteria.
Cultural Norms in India
In India, traditional and contemporary beauty ideals further complicate the landscape of body image. The cultural emphasis on certain physical attributes can intensify feelings of inadequacy among those who do not conform to these standards. This societal pressure contributes to the prevalence of body dysmorphic disorder and eating disorders, as individuals strive to meet culturally endorsed ideals.
Impact of Social Media
Social media platforms have become pervasive in modern society, especially among adolescents and young adults. While these platforms offer opportunities for connection and self-expression, they also present risks related to body image and mental health. Exposure to idealized and often unrealistic images can lead to negative self-comparisons, body dissatisfaction, and the internalization of narrow beauty ideals. This phenomenon is not limited to women; men are increasingly affected, with rising cases of muscle dysmorphia linked to media portrayals of the 'ideal' male physique.
Gender-Specific Pressures
Sociocultural influences on body image and related disorders often differ between genders. Women frequently face pressures to achieve thinness, leading to disorders like anorexia nervosa and bulimia nervosa. Conversely, men may experience pressure to attain muscularity, contributing to conditions such as muscle dysmorphia. These gender-specific pressures are perpetuated by media representations and cultural narratives that equate physical appearance with success and desirability.
Cultural Shifts and Globalization
Globalization has facilitated the exchange of cultural ideals, leading to shifts in beauty standards worldwide. In India, exposure to Western media has introduced new body ideals, often emphasizing slimness and specific body shapes. This shift can create a dissonance between traditional body ideals and contemporary expectations, exacerbating body dissatisfaction and contributing to the development of BDD and eating disorders.
Table: Sociocultural Factors Influencing BDD and Eating Disorders
|
Factor |
Description |
|
Media Representation |
Promotion of unattainable beauty standards through various media channels. |
|
Social Media Usage |
Increased exposure to curated and edited images leading to negative self-comparison. |
|
Cultural Beauty Ideals |
Societal emphasis on specific physical attributes as markers of beauty and success. |
|
Gender Norms |
Distinct pressures on men and women to conform to different body ideals. |
|
Globalization |
Introduction and internalization of foreign beauty standards, leading to cultural dissonance. |
Relationship Between Social Media Usage and Body Image Disturbance
Implications for Intervention
Addressing the sociocultural influences on BDD and eating disorders requires a multifaceted approach:
-
Media Literacy Education: Teaching individuals to critically evaluate media content can reduce the internalization of unrealistic beauty standards.
-
Promotion of Diverse Body Representations: Encouraging media platforms to showcase a variety of body types can help normalize diversity and reduce body dissatisfaction.
-
Cultural Sensitivity in Treatment: Understanding the cultural context is essential for developing effective interventions, particularly in diverse societies like India.
-
Gender-Inclusive Approaches: Recognizing and addressing the unique pressures faced by different genders can lead to more effective prevention and treatment strategies.
By acknowledging and addressing these sociocultural factors, mental health professionals, educators, and policymakers can work together to mitigate the impact of harmful beauty standards and support individuals struggling with body dysmorphic disorder and eating disorders.
Diagnostic Challenges in Co-occurring Body Dysmorphic Disorder and Eating Disorders
Accurately diagnosing co-occurring Body Dysmorphic Disorder (BDD) and eating disorders presents significant challenges due to overlapping symptoms, societal misconceptions, and the complex nature of both conditions. Understanding these challenges is crucial for developing effective assessment tools and treatment plans.
Symptom Overlap
Both BDD and eating disorders involve a preoccupation with body image, leading to behaviors such as excessive mirror checking, restrictive eating, and compulsive exercising. This overlap can make it difficult for clinicians to distinguish between the two disorders, potentially resulting in misdiagnosis or incomplete treatment plans. For instance, while BDD may focus on perceived flaws in specific body parts, eating disorders often center around weight and shape concerns. Recognizing these nuances is crucial for effective intervention.
Assessment Tools
To navigate these diagnostic complexities, healthcare professionals employ comprehensive assessment tools designed to evaluate the presence and severity of both disorders. Structured interviews, self-report questionnaires, and behavioral observations are utilized to gather detailed information about an individual's symptoms and their impact on daily functioning. Accurate diagnosis is essential, as the co-occurrence of BDD and eating disorders can exacerbate the severity of each condition, necessitating integrated treatment approaches.
Differential Diagnosis
Differentiating between BDD and eating disorders requires careful consideration of the primary concerns and behaviors associated with each condition. In BDD, the preoccupation is typically with a perceived defect in appearance, which may not be related to body weight or shape, such as concerns about facial features, skin imperfections, or hair. Conversely, eating disorders involve an intense fear of gaining weight and behaviors aimed at controlling body weight and shape, such as restrictive eating, bingeing, or purging. Understanding these distinctions is vital for accurate diagnosis and treatment planning.
Comorbidity and Its Implications
The co-occurrence of BDD and eating disorders is not uncommon and can complicate the clinical picture. Studies have shown that individuals with eating disorders may also exhibit symptoms of BDD, leading to more severe psychopathology and poorer treatment outcomes. This comorbidity necessitates a comprehensive assessment to identify all relevant symptoms and develop an integrated treatment plan that addresses both disorders simultaneously.
Cultural Considerations
Cultural factors play a significant role in the manifestation and perception of body image disturbances. In India, societal standards and traditional beliefs about body image can influence the presentation of BDD and eating disorders. Awareness of these cultural nuances is essential for clinicians to provide culturally sensitive assessments and interventions.
Implications for Treatment
Accurate diagnosis of co-occurring BDD and eating disorders is critical for effective treatment. Integrated therapeutic approaches that address both body image disturbances and disordered eating behaviors are recommended. Cognitive-behavioral therapy (CBT) has been shown to be effective in treating both conditions, focusing on challenging distorted beliefs about appearance and developing healthier coping strategies. In some cases, pharmacotherapy may also be considered as part of a comprehensive treatment plan.
The diagnostic challenges presented by the overlap of BDD and eating disorders require clinicians to employ thorough assessment strategies and maintain an awareness of the nuanced differences between the two conditions. By doing so, they can develop effective, individualized treatment plans that address the unique needs of each patient, ultimately improving outcomes and quality of life for those affected by these complex disorders.
Treatment Approaches for Co-occurring Body Dysmorphic Disorder and Eating Disorders
Addressing co-occurring Body Dysmorphic Disorder (BDD) and eating disorders necessitates a comprehensive, integrated treatment approach that considers the complex interplay between these conditions. Such an approach ensures that both disorders are treated concurrently, leading to more effective and lasting outcomes.
Integrated Therapy Models
Integrated therapy models are designed to address the multifaceted nature of co-occurring BDD and eating disorders. These models combine various therapeutic modalities to target the underlying cognitive and behavioral aspects of both conditions. By treating body dysmorphia and eating disorders simultaneously, integrated therapy models aim to reduce symptom severity and improve overall functioning.
Struggling with the connection between body dysmorphic disorder and eating disorders? Consulting an online psychologist in India or finding a psychologist near me can help address body image concerns and develop a healthier mindset.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a cornerstone in treating both BDD and eating disorders. This evidence-based approach focuses on identifying and challenging distorted thought patterns related to body image and self-worth. Through CBT, individuals learn to replace negative beliefs with healthier perspectives, leading to a reduction in compulsive behaviors associated with body dysmorphia and disordered eating. Studies have demonstrated the efficacy of CBT in addressing the core symptoms of both conditions, making it a vital component of integrated treatment plans.
Pharmacotherapy
In certain cases, medication may be prescribed to manage symptoms associated with BDD and eating disorders. Selective serotonin reuptake inhibitors (SSRIs) are commonly used to address underlying anxiety and depression, which often accompany these conditions. Pharmacotherapy should be closely monitored by healthcare professionals and is most effective when combined with psychotherapeutic interventions.
Family-Based Therapy
Family involvement is crucial, especially for adolescents dealing with BDD and eating disorders. Family-Based Therapy (FBT) empowers family members to support their loved one's recovery process. This approach fosters a supportive home environment, addresses dysfunctional family dynamics, and educates family members about the disorders, enhancing the overall treatment outcome.
Mindfulness and Acceptance-Based Therapies
Mindfulness practices, such as Mindfulness-Based Cognitive Therapy (MBCT) and Acceptance and Commitment Therapy (ACT), have shown promise in treating BDD and eating disorders. These therapies encourage individuals to develop a non-judgmental awareness of their thoughts and feelings, reducing the impact of negative body image and promoting healthier relationships with food and appearance.
Nutritional counselling
Registered dietitians play a vital role in the treatment team by providing nutritional counselling tailored to the individual's needs. This includes developing balanced meal plans, educating about proper nutrition, and addressing any misconceptions related to food and body image. Nutritional counselling helps restore physical health and establishes a healthier relationship with food.
Support Groups and Peer Support
Engaging in support groups provides individuals with a sense of community and shared experience. Peer support offers emotional encouragement, reduces feelings of isolation, and allows for the exchange of coping strategies. Support groups can be a valuable adjunct to formal therapy, fostering a sense of belonging and understanding.
Holistic Approaches
Incorporating holistic approaches, such as art therapy, yoga, and meditation, can complement traditional treatments. These modalities promote self-expression, reduce stress, and enhance overall well-being, contributing to a more comprehensive recovery process.
Challenges in Treatment
Treating co-occurring BDD and eating disorders presents unique challenges, including:
-
Diagnostic Overlap: The similarity in symptoms can complicate accurate diagnosis, necessitating thorough assessments by experienced clinicians.
-
Resistance to Treatment: Individuals may be ambivalent about treatment due to fear of weight gain, change in appearance, or confronting deep-seated beliefs.
-
Comorbid Conditions: The presence of additional mental health issues, such as depression or anxiety disorders, requires integrated treatment plans that address all coexisting conditions.
A multifaceted and individualized treatment approach is essential for effectively addressing co-occurring Body Dysmorphic Disorder and eating disorders. By integrating various therapeutic modalities and involving a multidisciplinary team, individuals can achieve a more comprehensive and sustained recovery, leading to improved quality of life and well-being.
Case Studies and Testimonials
Real-life experiences provide valuable insights into the challenges and triumphs of individuals dealing with both Body Dysmorphic Disorder (BDD) and eating disorders. These narratives highlight the importance of comprehensive treatment approaches and offer hope to those facing similar struggles.
Real-Life Experiences
Case Study: Differentiating BDD from Eating Disorders
A 20-year-old woman was admitted to a disordered eating unit due to significant weight loss and restrictive eating behaviors. Initially suspected of having anorexia nervosa, she disclosed a long-standing preoccupation with perceived facial flaws, leading to a diagnosis of BDD and avoidant/restrictive food intake disorder (ARFID). This case underscores the necessity of distinguishing between body dysmorphia and distorted body image associated with eating disorders, as treatment approaches differ for each condition.
Testimonial: Overcoming Muscle Dysmorphia
George Mycock, a university student from Stoke-on-Trent, suffered from muscle dysmorphia, a subtype of BDD characterized by an obsession with not being muscular enough. This condition led him to severe depression and suicidal thoughts. Triggered by an early childhood injury that resulted in weight gain, George's struggle with achieving the 'perfect' muscular body led to a cycle of compulsive training, binge eating, and self-loathing. His recovery was facilitated by friends' intervention and support, leading him to found MyoMinds, an organization helping others with muscle dysmorphia and BDD. George's story highlights the rising concern of body image issues among young men, driven by media representation of unrealistic body standards.
Testimonial: Navigating Social Media Influences
Indya, a teenager from Adelaide, developed anorexia at the age of 13, influenced by social media fitness trends promoting the 'perfect' body. She engaged in popular online workouts, which, combined with pandemic-induced isolation, exacerbated her condition. Misunderstood and misdiagnosed due to her appearance, her health deteriorated until she received specialized care. Now 19, Indya advocates for better treatment options and emphasizes the need for content moderation on social media platforms to prevent the exacerbation of eating disorders among young people.
Case Study: Olympic Athlete's Struggle
Levi Jung-Ruivivar, an 18-year-old Olympic gymnast, publicly shared her battle with an eating disorder that significantly impacted her mental and physical well-being. Representing the Philippines at the 2024 Paris Olympics, Levi decided to take a leave of absence from Stanford University to focus on her recovery. Her openness aims to destigmatize eating disorders and encourage others facing similar challenges to seek help.
Expert Commentary
Dr. Anjali Mehta, a leading psychologist specializing in body image disorders, emphasizes the necessity of addressing both conditions concurrently. She notes, "The intertwined nature of body dysmorphic disorder and eating disorders requires a holistic treatment plan. By focusing on the cognitive distortions and behavioral patterns common to both, we can facilitate more effective recovery outcomes."
Implications for Treatment
These case studies and testimonials underscore the importance of integrated treatment approaches in managing co-occurring BDD and eating disorders. Key considerations include:
-
Comprehensive Assessment: Accurate diagnosis is crucial, as overlapping symptoms can lead to misdiagnosis. Differentiating between BDD and eating disorders ensures that treatment plans address the specific needs of the individual.
-
Integrated Therapeutic Approaches: Combining cognitive-behavioral therapy (CBT) with other modalities, such as mindfulness-based interventions and family-based therapy, can address the multifaceted nature of these disorders.
-
Awareness and Education: Educating patients, families, and healthcare providers about the coexistence of BDD and eating disorders can lead to earlier intervention and improved outcomes.
-
Support Systems: Encouraging participation in support groups and peer networks provides individuals with a sense of community and shared experience, which can be instrumental in the recovery process.
Real-life experiences and expert insights highlight the complex relationship between body dysmorphic disorder and eating disorders. Integrated, individualized treatment approaches are essential for effective management and recovery. By learning from individual experiences and professional expertise, we can better understand and address the complexities of these intertwined conditions.
Resources and Support Systems for Body Dysmorphic Disorder and Eating Disorders in India
Navigating the challenges of Body Dysmorphic Disorder (BDD) and eating disorders necessitates access to comprehensive resources and support systems. In India, a range of professional services, support groups, and educational materials are available to assist individuals on their path to recovery.
Understanding Body Dysmorphic Disorder and Eating Disorders
Body Dysmorphic Disorder is a mental health condition characterized by an obsessive focus on perceived flaws in one's appearance, which may be minor or unobservable to others. This preoccupation can lead to significant distress and impair daily functioning. Eating disorders, such as anorexia nervosa, bulimia nervosa, and binge eating disorder, involve unhealthy relationships with food and body image, often resulting in severe physical and psychological consequences.
Professional Help
Seeking guidance from qualified professionals is a crucial step toward recovery. In India, several organizations and platforms offer specialized services:
-
Medicover Hospitals: Provides access to psychiatrists and psychologists experienced in treating BDD and eating disorders. Their approach includes cognitive-behavioral therapy, medication management, and supportive care aimed at enhancing self-esteem and managing symptoms.
-
Samarpan Health Centre, Mumbai: Offers comprehensive treatment for eating disorders, encompassing mental health counselling, therapy sessions, group therapy, medication management, psychiatric consultations, and nutritional counselling. Their multidisciplinary team collaborates to create personalized treatment plans addressing the unique needs of each individual.
Support Groups
Engaging with support groups provides emotional reinforcement and a sense of community. Sharing experiences with others facing similar challenges can alleviate feelings of isolation and promote healing:
-
Body Dysmorphic Disorder Foundation: Hosts online support groups accessible worldwide, including participants from India. These user-led groups offer opportunities to connect, share experiences, and provide mutual support. Meetings are held via Zoom, with schedules accommodating various time zones.
-
Overeaters Anonymous (OA): A twelve-step program supporting individuals with problematic relationships with food, including those dealing with binge eating, bulimia, and anorexia. OA offers meetings in over 75 countries, with options for in-person, phone, and online gatherings. While OA is not specific to BDD, it provides support for related eating issues.
Educational Resources
Access to accurate information is vital for understanding and managing these conditions:
-
National Eating Disorders Association (NEDA): Offers comprehensive resources on eating disorders, including definitions, symptoms, and treatment options. While based in the USA, NEDA's online materials are accessible globally and provide valuable insights applicable in various contexts.
-
HelpGuide.org: Provides detailed information on Body Dysmorphic Disorder, including symptoms, causes, and treatment approaches. This resource aids in understanding the complexities of BDD and offers guidance on seeking appropriate help.
Table: Resources for Support
|
Organization |
Services Offered |
Contact Information |
|
Medicover Hospitals |
counselling and Therapy |
Website |
|
Samarpan Health Centre, Mumbai |
Comprehensive Eating Disorder Treatment |
Website |
|
Body Dysmorphic Disorder Foundation |
Online Support Groups |
Website |
|
Overeaters Anonymous |
Support Meetings for Eating Issues |
Website |
Accessing Support
Taking the first step toward seeking help can be daunting, but numerous resources are available to support individuals dealing with BDD and eating disorders in India:
-
Online Directories: Platforms like the Indian Psychiatric Society offer directories of certified mental health professionals across the country, enabling individuals to find experts tailored to their needs.
-
Helplines: Organizations such as FindaHelpline provide information on eating and body image helplines in India, offering immediate support and guidance.
Navigating the complexities of Body Dysmorphic Disorder and eating disorders requires a multifaceted approach, encompassing professional treatment, peer support, and educational resources. In India, a variety of avenues are available to assist individuals on their journey toward recovery. By leveraging these resources, those affected can find the support necessary to manage their conditions and improve their quality of life.
Conclusion
Understanding the intricate connection between Body Dysmorphic Disorder (BDD) and eating disorders is vital for effective diagnosis and treatment. Both conditions share overlapping psychological factors, such as body image disturbances and perfectionism, which can exacerbate the severity of each disorder. Recognizing these shared elements allows for the development of integrated therapeutic approaches, addressing the root causes and promoting holistic recovery.
Integrated Therapeutic Approaches
The co-occurrence of BDD and eating disorders necessitates a comprehensive treatment strategy that simultaneously addresses both conditions. Cognitive Behavioral Therapy (CBT) has been identified as a cornerstone in treating these disorders. CBT focuses on identifying and challenging distorted thought patterns related to body image and self-worth, enabling individuals to replace negative beliefs with healthier perspectives. This approach has demonstrated efficacy in reducing compulsive behaviors associated with both BDD and eating disorders.
In addition to CBT, pharmacotherapy may be considered, particularly when symptoms are severe or unresponsive to psychotherapy alone. Selective Serotonin Reuptake Inhibitors (SSRIs) are commonly prescribed to manage underlying anxiety and depression, which often accompany these conditions. A multidisciplinary approach, involving mental health professionals, dietitians, and medical practitioners, ensures that all aspects of the disorders are addressed, promoting a more robust recovery process.
Sociocultural Influences
Sociocultural factors significantly influence the development and maintenance of BDD and eating disorders. The pervasive portrayal of idealized body types in media and social platforms contributes to body image dissatisfaction. Studies have shown that increased exposure to social media correlates with heightened body dissatisfaction and the development of disordered eating behaviors. This is particularly evident among adolescents and young adults, who are more susceptible to internalizing these unrealistic standards.
In the Indian context, traditional beauty standards and cultural norms further shape perceptions of body image. A comprehensive review examining body image dissatisfaction in rural India highlighted the multifaceted factors influencing individual perceptions and societal expectations. The study emphasized the complex interplay between cultural nuances, economic disparities, and gender-specific experiences, underscoring the need for culturally sensitive mental health interventions.
Professional Help and Support Systems
For individuals affected by BDD and eating disorders, seeking professional help is paramount. In India, various resources and support systems are available to assist in the recovery journey. The Indian Psychiatric Society offers a directory of certified professionals across the country, facilitating access to qualified mental health experts. Additionally, online platforms such as FindaHelpline provide information on eating disorder and body image helplines in India, offering immediate support and guidance.
Engaging with support groups can also provide emotional reinforcement and a sense of community. Sharing experiences with others facing similar challenges can alleviate feelings of isolation and promote healing. While some support groups are based internationally, many offer online sessions accessible to individuals worldwide, including those in India.
Table: Resources for Support
|
Organization |
Services Offered |
Contact Information |
|
Indian Psychiatric Society |
Directory of Certified Mental Health Professionals |
Website |
|
FindaHelpline |
Eating Disorder and Body Image Helplines |
Website |
|
Body Dysmorphic Disorder Foundation |
Online Support Groups |
Website |
|
Overeaters Anonymous |
Support Meetings for Eating Issues |
Website |
Addressing Body Dysmorphic Disorder and eating disorders requires a multifaceted approach that encompasses understanding, professional intervention, and societal change. By acknowledging the complexities of these intertwined conditions and leveraging available resources, individuals can embark on a path toward healing and improved well-being. It is imperative to foster awareness and critical evaluation of sociocultural influences, develop integrated therapeutic strategies, and ensure accessible support systems to effectively combat these pervasive disorders.
FAQs
1. How are Body Dysmorphic Disorder (BDD) and Eating Disorders related?
BDD and eating disorders both involve significant preoccupations with body image, but they differ in focus. Individuals with eating disorders often have a distorted perception of their body weight and shape, leading to behaviors aimed at weight control. In contrast, those with BDD are preoccupied with perceived flaws in specific body parts, which may not be related to weight or shape. Despite these differences, both conditions can coexist, and understanding their distinctions is crucial for effective treatment.
2. Can social media contribute to the development of BDD and Eating Disorders?
Yes, social media can play a significant role in the development and exacerbation of both BDD and eating disorders. Platforms that emphasize appearance and beauty standards can lead to increased body dissatisfaction and unhealthy comparison. Exposure to idealized images and societal pressures online may contribute to the onset of these disorders.
3. What are the warning signs of BDD and Eating Disorders?
Early recognition of BDD and eating disorders is vital. Common warning signs include:
-
BDD:
-
Excessive mirror checking or avoidance
-
Preoccupation with perceived physical flaws
-
Frequent cosmetic procedures without satisfaction
-
Avoidance of social situations due to appearance concerns
-
Eating Disorders:
-
Preoccupation with food, dieting, and body weight
-
Dramatic weight loss or fluctuations
-
Withdrawal from social activities involving food
-
Engaging in purging behaviors or excessive exercise
If you or someone you know exhibits these signs, seeking professional help is essential.
4. What treatments are available for BDD and Eating Disorders?
Effective treatment often involves a multidisciplinary approach:
-
Cognitive Behavioral Therapy (CBT): Addresses distorted thoughts and behaviors related to body image and eating habits.
-
Medication: Selective Serotonin Reuptake Inhibitors (SSRIs) may be prescribed to manage underlying anxiety and depression associated with these disorders.
-
Nutritional counselling: Guidance from dietitians to establish healthy eating patterns and address nutritional deficiencies.
-
Support Groups: Connecting with others facing similar challenges can provide emotional support and coping strategies.
Early intervention and a comprehensive treatment plan tailored to the individual's needs are crucial for recovery.
5. Can BDD and Eating Disorders be cured?
While there is no definitive "cure," many individuals recover and lead fulfilling lives with appropriate treatment. Recovery involves managing symptoms, addressing underlying issues, and developing healthy coping mechanisms. Ongoing support and therapy play significant roles in maintaining progress and preventing relapse.
6. Where can I seek help for BDD and Eating Disorders in India?
Several organizations in India offer support and treatment:
-
Indian Psychiatric Society: Provides a directory of certified mental health professionals across the country.
-
FindaHelpline: Offers information on eating disorder and body image helplines in India.
-
Body Dysmorphic Disorder Foundation: Hosts online support groups accessible to individuals worldwide, including those in India.
Reaching out to these resources can provide the necessary guidance and support for recovery.
Understanding BDD and eating disorders is the first step toward effective intervention and recovery. If you or someone you know is struggling with these conditions, seeking professional help is crucial. With the right support and treatment, individuals can work towards healing and leading a balanced life.
Transform Your Life with Expert Guidance from Click2Pro
At Click2Pro, we provide expert guidance to empower your long-term personal growth and resilience. Our certified psychologists and therapists address anxiety, depression, and relationship issues with personalized care. Trust Click2Pro for compassionate support and proven strategies to build a fulfilling and balanced life. Embrace better mental health and well-being with India's top psychologists. Start your journey to a healthier, happier you with Click2Pro's trusted online counselling and therapy services.






